Introduction
The jugular bulb (JB) is the venous bulbous enlargement between the sigmoid sinus and the internal jugular vein. The JB is known to develop with age. Immediately after birth, the JB is not recognizable as an anatomical structure, but it develops after 2 years., Size and morphology of the JB vary widely among individuals, some of which are diagnosed as JB abnormalities, such as high riding jugular bulb (HRJB), dehiscent JB, and protruding JB. These JB abnormalities may cause conductive hearing loss, pulsatile tinnitus, and vertigo. Although there are no definitive criteria for the diagnosis of HRJB, HRJB is commonly diagnosed when the superior edge of JB reaches the level of the internal auditory canal (IAC), based on the results of the previous study comparing histopathologic and CT imaging findings. Previous studies reported that the frequency of JB abnormalities increases with age. Focusing on the prevalence of HRJB in different age groups, HRJB is found in only 1.7% of the population in the first decade of life. However, this prevalence increases with age to approximately 10% until age 50, after which it remains constant.
The dehiscence of the JB, the bony wall defect between the JB and surrounding structures such as the middle ear, is relatively rare among the JB abnormalities. Due to the lack of the bony wall, the HRJB with dehiscence can protrude into the tympanic cavity, forming a diverticulum, leading to a high risk of hemorrhagic complications during middle ear surgeries. The dehiscence of the JB can be observed with or without HRJB. According to the retrospective radiologic study reviewing 1010 patients of any ear symptom, the incidence of dehiscent JB and dehiscent HRJB is reported as 7.5% and 2%, respectively. There are few case reports of HRJB protruding into the tympanic cavity in children., Although there is a case report of an adult in which the dehiscent HRJB protruding into the middle ear cavity had progressed, there have been no reports about how the HRJB has become dehiscent to and protruded into the middle ear cavity.
We herein report a case of congenital deaf child who had the HRJB without dehiscence very early in his life, at the age of nine months. The CT images at the age of 6 years revealed that the HRJB increased in size and protruded into the middle ear cavity through the bony wall dehiscence. This is the first reported pediatric case whose longitudinal CT images demonstrate that the bony wall of the HRJB disappears to develop a diverticulum protruding into the tympanic cavity as the age increases.
Case Report
A 1 year and three months old boy with bilateral profound hearing loss was referred to our hospital for cochlear implantation (CI). His newborn hearing screening tests were positive, and the subsequent ABR examination showed no responses at 105 dBHL bilaterally. He was fitted with hearing aids in both ears from five months of age, but no apparent auditory response was observed. At nine months, temporal bone CT images revealed bilateral inner ear malformation showing cystic cochleas without modiolus, categorized as incomplete partition type I (IP-I) based on Sennaroglu’s classification. CT images also showed a lack of bony septum between IP-I and the IAC in both ears. Furthermore, T2-weighted MRI revealed that the bilateral cystic cochleas were thoroughly connected to the IAC, implying that the intracranial pressure was transmitted from the IAC into the malformed inner ear. In contrast to these left–right symmetrical findings, cochlear nerve deficiency (CND) was evident on the right side, although the left cochlear nerve was well depicted (Figure 1). These results suggested the high risk of cerebrospinal fluid (CSF) gusher during CI at both sides and poorer cochlear implant outcomes on the right side than the left side. His JB was enlarged only on the right side, and its axial section area at the level of the round window (RW) was 0.44 cm2 (Figure 2). We calculated the area by approximating JB as an ellipse. CT images also demonstrated that the superior margin of the right JB reached the level of IAC, meeting the criteria for HRJB (Figure 1). The right HRJB was facing the tympanic cavity at the tympanic sinus, but appeared to be covered by a thin bony wall and did not protrude into the middle ear (Figure 2).
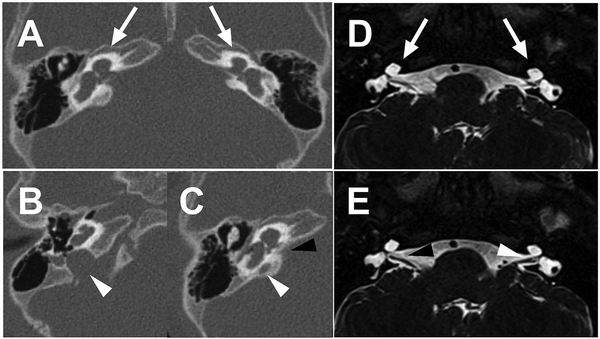
Figure 1
A, B, C: axial CT images at nine months. D, E: axial MRI images at eighteen months. A, B, C: At nine months, axial CT images reveal an inner ear malformation, IP-I on both ears (arrows) and HRJB on the right ear (white arrowhead). At the level of the IAC (black arrowhead), the JB (white arrowhead) can also be seen, meeting the criteria of HRJB at nine months. D and E: axial T2-weighted MRI demonstrates that the bilateral cystic cochleas are thoroughly connected to the IAC (arrows). The normal diameter of the left cochlear nerve is shown (white arrowhead), while in the right ear, the cochlear nerve is hypoplastic or aplastic, indicating CND (black arrowhead).
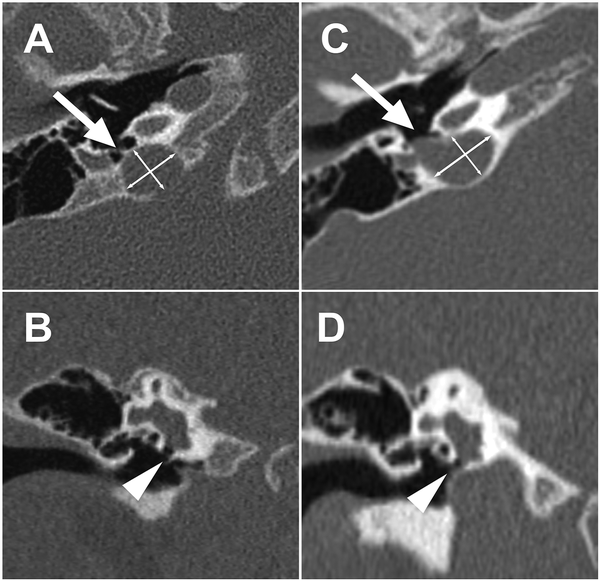
Figure 2
A, B: CT images at nine months. C, D: CT images at six years. A and C: Axial CT images at the level of the round window (RW) at nine months and 6 years, respectively. The area of JB at 9 months and 6 years are 0.44 cm2 (A) and 0.59 cm2 (C), respectively. The vascular wall of HRJB is covered by a thin bony wall at nine months (A, arrow), but the bony wall between the HRJB and the middle ear cavity is absent at 6 years (C, arrow). The diverticulum protrudes through the dehiscence of HRJB and occupies the tympanic sinus at 6 years. B and D: Coronal CT images at the level of the RW at 9 months and 6 years, respectively. The height of JB is increased, and the RW is covered at six years (D, arrowhead).
He underwent left cochlear implantation at the age of 19 months. We performed cochleostomy for electrode insertion because the RW was hypoplastic. A CSF gusher occurred immediately after cochleostomy but was stopped by packing soft tissue around the electrode. His postoperative auditory performance using the cochlear implant was good, and his monosyllabic word discrimination scores with the left cochlear implant reached 85% at five years. Before entering the elementary school at 6 years, his parents wanted him to receive second CI on his right ear to achieve binaural hearing. Therefore, another temporal bone CT scan was conducted for preoperative evaluation. Surprisingly, this CT scan demonstrated that the right HRJB had enlarged and become dehiscent to the middle ear cavity. The axial section area of the right HRJB at the level of the RW was 0.59 cm2 (Figure 2). This dehiscent HRJB had protruded into the tympanic cavity, forming the diverticulum occupying the tympanic sinus and covering the RW (Figure 2). Based on this CT scan, we decided not to proceed with the cochlear implantation on the right side.
Discussion
Previous anatomical and radiographic studies reported that the JB usually develops more than two years after birth., However, the present case already had the HRJB reaching the level of the IAC at nine months. We found only one published report of HRJB in a child younger than two years of age, suggesting that HRJB is very rare in children younger than one year. Furthermore, when this patient was six-years-old, the HRJB had enlarged and was accompanied by a defect in the bony wall and a diverticulum protruding into the middle ear cavity. This is the first case report to show the longitudinal CT study, demonstrating that an HRJB can exist in infancy and grow over to protrude into the middle ear cavity.
The mechanism of HRJB development is unrevealed. However, it is assumed that the amount of blood in the venous system, the upward forces on JB originating from the heart, and the enlargement of mastoid pneumatization are associated with HRJB development. The cross-sectional epidemiological studies have reported that the frequency of HRJB increases with age. The axial section area of the HRJB also showed a trend to increase with age. Thus, it seems that, at least, aging is an essential factor in the development and enlargement of JB. To accurately examine the effect of age on HRJB, longitudinal epidemiological studies, rather than cross-sectional studies, are needed to see how the morphology and size of HRJB change with aging. However, no such longitudinal study has been published.
Since the present case exhibited HRJB at nine months of age, factors causing the formation of JB, probably the continuous veinous blood flow and pressure, may have worked very early during the childhood. These factors may also have caused subsequent enlargement of the HRJB. The longitudinal imaging results of the present case prove that the HRJB enlarges as age increases and suggest that the earlier the HRJB forms, the larger the HRJB may grow. It should also be noted that the present case showed no apparent dehiscence on the bony surface of the HRJB at the age of nine months, while a diverticulum had protruded from a defect of the bony wall of the HRJB into the middle ear cavity at the age of six years. These results mean that the diverticulum and dehiscence of the HRJB were not congenital in this case. As the HRJB increases in size, the bony wall covering the HRJB may have been stretched thin, resulting in subsequent dehiscence of the bony wall and protrusion of the vessel wall from the dehiscence.
It is well known that the HRJB with a diverticulum protruding into the tympanic cavity has a high risk of significant bleeding during middle ear surgeries. However, there are few reports of CI in patients with HRJB with a diverticulum covering the RW. Therefore, it is difficult to accurately predict the possible complications of CI in the present case. In particular, since this case had severe cochlear malformations, the risk of electrode displacement and recurrent CSF gusher after surgery, in addition to massive bleeding during surgery, should be considered. Given that the RW was hypoplastic on the left side (the first CI side), cochleostomy would also be required in the right ear. However, since the right protruding HRJB covered the RW niche, it should be challenging to expose the RW and perform cochleostomy safely. Even if the electrode could be inserted without any trouble, there is still a postoperative risk that the expanding diverticulum will expand further to push the inserted electrodes laterally, causing an electrode slip-out and/or a recurrent CSF gusher from the cochleostomy site. Since MRI revealed CND on the right side, auditory performance using the right cochlear implant was expected poorer than that with the left cochlear implant. Thus, we decided not to perform the CI on the right side because of the high risks associated with the surgery and the limited benefits.
In this case, the cross-sectional area of the HRJB had increased in 6 years, and the protruding diverticulum newly emerged. These findings suggest that in the future, the diverticulum of his right HRJB may grow further, touching the eardrum or protruding into the ear canal. Thus, we will continue to evaluate the size and morphology of the HRJB in this case by using CT scans. If the diverticulum is growing rapidly, some surgery may be needed to suppress its rate of growth. Resurfacing the HRJB with bone cement was reported effective to stop tinnitus caused by the HRJB. This surgical technique may also be useful to suppress the growth rate of the HRJB with the diverticulum.
Conclusion
We experienced a congenitally deaf child with an inner ear malformation who already had the HRJB very early in his life, at nine months. At six years, the HRJB had enlarged, and a diverticulum from the HRJB emerged to protrude into the middle ear cavity and cover the RW. This longitudinal CT study proves that the HRJB can enlarge with age, and suggests that the earlier the HRJB forms, the larger the HRJB may grow. The HRJB in children under two years of age is extremely rare and requires careful assessment in determining the indications for otologic surgery. The early developed HRJB may enlarge and be associated with a diverticulum that can cause massive bleeding during surgeries. Furthermore, in exceptional cases such as cochlear implant candidates with severe inner ear malformations, we must consider possible complications such as CSF gushers and electrode array displacement that the continuously growing HRJB may cause.
Acknowledgments
The authors would like to thank Dr Syo Koyasu for useful discussions.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work is supported by KAKENHI Grant-in-Aid for Scientific Research (C) JP20K09709 (H.Y.), JP18K09392(Y.N.).
References
- 1. Friedmann DR, Eubig J, McGill M, Babb JS, Pramanik BK, Lalwani AK. Development of the jugular bulb: a radiologic study. Otol Neurotol. 2011;32:1389–1395.
- 2. Okudera T, Huang YP, Ohta T, et al. Development of posterior fossa dural sinuses, emissary veins, and jugular bulb: morphological and radiologic study. Am J Neuroradiol. 1994;15:1871–1883.
- 3. Friedmann DR, Eubig J, Winata LS, et al. A clinical and histopathologic study of jugular bulb abnormalities. Arch Otolaryngol Head Neck Surg. 2012;138:66–71.
- 4. Friedmann DR, Eubig J, Winata LS, Pramanik BK, Merchant SN, Lalwani AK. Prevalence of jugular bulb abnormalities and resultant inner ear dehiscence: A histopathologic and radiologic study. Otolaryngol-Head Neck Surg (Tokyo). 2012;147:750–756.
- 5. Shihada R, Maimon S, Braun J, Fradis M, Luntz M. Endovascular embolization of a hemorrhagic jugular bulb diverticulum. Int J Pediatr Otorhinolaryngol. 2008;72:1445–1448.
- 6. Atmaca S, Elmali M, Kucuk H. High and dehiscent jugular bulb: Clear and present danger during middle ear surgery. Surg Radiol Anat. 2014;36:369–374.
- 7. Kuhn MA, Friedmann DR, Winata LS, et al. Large jugular bulb abnormalities involving the middle ear. Otol Neurotol. 2012;33:1201–1206.
- 8. Sennaroglu L. Cochlear implantation in inner ear malformations--a review article. Cochlear Implants International. 2010;11:4–41.
- 9. Yamazaki H, Leigh J, Briggs R, Naito Y. Usefulness of MRI and EABR testing for predicting CI outcomes immediately after cochlear implantation in cases with cochlear nerve deficiency. Otol Neurotol. 2015;36:977–984.
- 10. Di Lella F, Falcioni M, Piccinini S, et al. Prevention and management of vascular complications in middle ear and cochlear implant surgery. Eur Arch Oto-Rhino-Laryngol. 2017;274:3883–3892.
- 11. Lee S-Y, Song S-K, Park SJ, et al. Jugular bulb resurfacing with bone cement for patients with high dehiscent jugular bulb and ipsilateral pulsatile tinnitus. Otol Neurotol. 2019;40:192–199.
