Backgrounds
The most common cause of sleep-disordered breathing symptoms (snoring, sleep apnea, nasal obstruction, or mouth breathing) in children is adenoid hypertrophy; adenoidectomy is one of the most curative operations, which is widely used in clinical practice., Torus tubarius hypertrophy (TTH) after adenoidectomy is rare reported, and its etiology and treatment is still unclear., In this article, we described the clinical features of TTH and shared some experiences about clinical treatments for TTH.
Material and Methods
Study Design
The present retrospective review was conducted from January 2017 to 2023 at the Children’s Hospital of Nanjing Medical University (Nanjing, China). A total number of 36 pediatric patients with TTH were identified at our institution. All of them met the following inclusion criteria: (1) have taken adenoidectomy before, (2) recurred sleep-disordered breathing symptoms over 3 months after surgery, (3) TTH confirmed by nasal endoscopy, and (4) absence of other systemic diseases. All 36 cases underwent 1-month conservative treatment period with intranasal corticosteroids and oral leukotriene receptor antagonist, if the sleep-disordered breathing symptoms did not improve, then partial resection of TTH was performed under general anesthesia.
Data Collection
For each case, patient age, sex, AR, time of first operation, time of TTH, time of partial resection of TTH, treatments, and outcomes were recorded.
Statistical Analysis
Data were statistically analyzed using the statistical software SPSS 26.0. Categorical variable are expressed as mean ± SD or median if not normally distributed. The Chi-square test was used for the comparison of categorical variables; the P-value < .05 was considered statistically significant.
Results
A total number of 36 pediatric patients with TTH were identified at the Children’s Hospital of Nanjing Medical University from January 2017 to 2023. The incidence of TTH in our institution is about 0.18% (the total number of adenoidectomy from January 2017 to 2023 is about 20,000 cases).
Demographics
Of the 36 patients with TTH, 27 were boys (75.0%) and 9 were girls (25.0%). The mean age of first operation was 42.31 ± 11.54 months (range 20-63 months); most of the cases were ≤5 years old (94.4%, n = 34).
Time of TTH
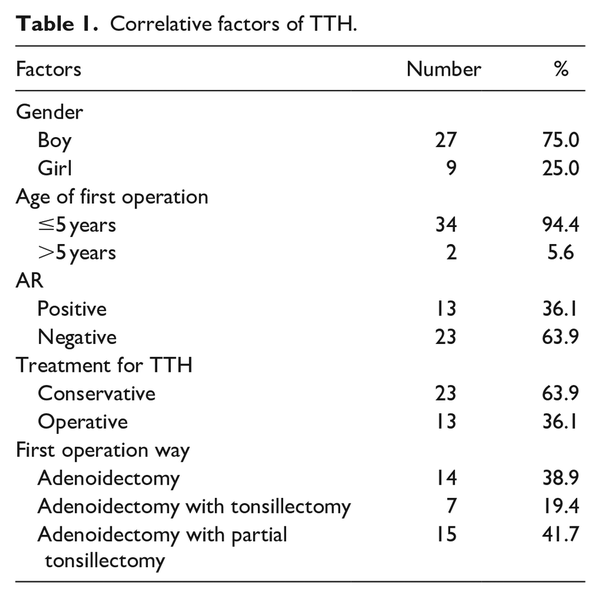
All patients with TTH were diagnosed by nasal endoscopy; the TTH blocked more than 1/2 posterior naris and caused sleep-disordered breathing symptoms (Figures 1 and 2), and the time interval between first operation and TTH ranged from 3 to 55 months.
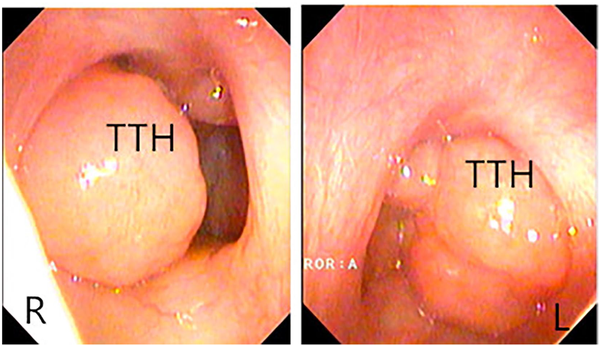
Figure 1
TTH diagnosed by nasal endoscopy.
Torus tubarius hypertrophy (TTH) blocks postnaris over ½.
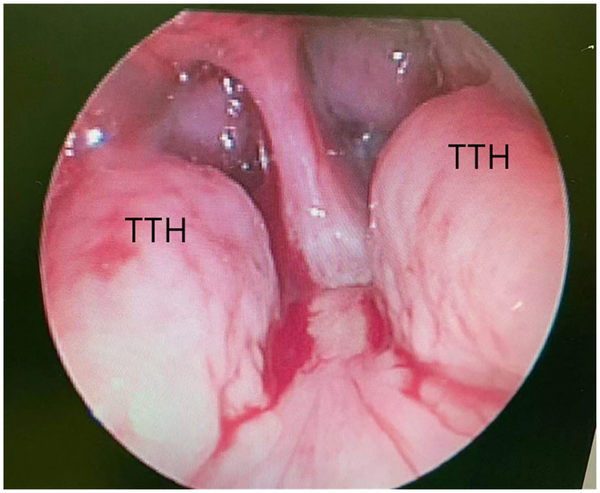
Figure 2
TTH viewed by 70° nasopharyngeal endoscopy.
Torus tubarius hypertrophy (TTH) blocks nasopharynx over ½.
Management and Outcome
Twenty-three patients’ symptoms were relieved by using intranasal corticosteroids and oral leukotriene receptor antagonist significantly; coblator-assisted partial resection of TTH was performed in 13 cases whose symptoms were not relieved by conservative treatment. All the patients were followed up from 6 months to 4 years; no patient had recurred sleep-disordered breathing symptoms for now, and no other therapy for TTH.
Patient with AR
Of the 36 patients with TTH, 13 had definite symptoms and signs of AR (36.1%).
First Operation Way
Of the 36 patients, 14 underwent adenoidectomy, 7 underwent adenoidectomy with tonsillectomy, and 15 underwent adenoidectomy with partial tonsillectomy. All the 36 operations were conducted by a low-temperature plasma technique under general anesthesia.
Correlative Factors of TTH
All the correlative factors (sex, time of first operation, AR, treatment of TTH, and first operation way) are presented in Table 1.
Discussion
Kim et al. first reported TTH after adenoidectomy in children; they also reported in preview articles that hypertrophy of the tubal tonsil might be TTH., The torus tubarius is the projecting posterior lip of the pharyngeal opening of the Eustachian tube, which forms the lateral border of nasopharynx. Tubal tonsil and torus tubarius are very close in anatomy; some studiers call them TTH., In this article, we introduce TTH as follows.
TTH and Demographics
Of all the 36 patients, TTH occurred in 27 boys (75.0%) and 9 girls (25.0%); 34 patients were younger than 5 years (94.4%). The results are consistent with preview studies., Kim et al. reported 7 children with TTH; all of them were boys, and all were younger than 5 years when they took the adenoidectomy. Yang et al. reported 11 patients with TTH; 10 of them (90.9%) were younger than 5 years when they took the adenoidectomy, but they did not mention the gender. We believed that TTH was more likely to happen in boys and in patients who took adenoidectomy before the age of 5 years.
AR and TTH
Preview articles indicated that adenoidal hypertrophy was associated with AR; the AR patients were more likely to have adenoidal hypertrophy.- They confirmed that about 21.2% to 46.4% AR patients had adenoidal hypertrophy, and about 13.6% to 44.9% patients with adenoidal hypertrophy had AR., Does AR also affect TTH? In this article, 13 of 36 children had AR (36.1%), which is consistent with Kim et al.’s results; in their article, 4 of 11 patients had AR (36.36%). The relationship between TTH and AR still needs more proofs.
Treatment for TTH
Many articles had proved that intranasal corticosteroids and oral leukotriene receptor antagonists can relieve or cure the symptoms of adenoid hypertrophy.- In our study, intranasal corticosteroids and oral leukotriene receptor antagonist can also relieve or cure the symptoms of TTH; only 13 patients underwent partial resection of TTH. Whether TTH has glucocorticoid receptors or leukotriene receptors needs more proofs. Unfortunately, no pathological examination of TTH was performed in our study.
First Operation and TTH
Does the first operation way affect TTH? 2052 patients who underwent adenoidectomy were randomly selected from our department from 2017 to 2019; 1225 patients took adenoidectomy with or without partial tonsillectomy, and 827 patients took adenoidectomy with tonsillectomy. In our study, 29 patients who underwent adenoidectomy with or without partial tonsillectomy had TTH; only 7 patients who underwent adenoidectomy with tonsillectomy had TTH. The Chi-square test shows that operation way affects TTH (P = .011). We think the (partial) tonsil could promote TT (torus tubarius) growth after adenoidectomy.
Limitations
Some limitations to this study need to be acknowledged. First, we do not know the percentage of AR patients undergoing adenoidectomy in our institution, so we could not know whether AR affects TTH. Second, we did not do nasal endoscopy for all patients after adenoidectomy, so we could miss some asymptomatic TTH.
Conclusion
TTH is a rare complication after adenoidectomy (0.2%), which tends to happen more in male pediatric patients and in patients who took adenoidectomy before the age of 5 years. Intranasal corticosteroid combined with oral leukotriene receptor antagonist is a helpful treatment. We also find that AR and the operation way might affect TTH. We advise that male patients aged less than 5 years with sleep-disorder symptoms should take adenoidectomy with tonsillectomy together and partial resection of TT to prevent TTH after surgery, and AR patients should take intranasal corticosteroids with oral leukotriene receptor antagonist about 1 month to prevent TTH after surgery.
Data Availability Statement The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Statements I certify that this manuscript is original and has not been published and will not be submitted elsewhere for publication while being considered by EAR, NOSE & THROAT JOURNAL. And the study is not split up into several parts to increase the quantity of submissions and submitted to various journals or to one journal over time. No data have been fabricated or manipulated (including images) to support my conclusions. No data, text, or theories by others are presented as if they were our own.
Xiao-Fei Shen
https://orcid.org/0000-0001-8782-2629
References
- 1. Passàli D, De BM, Lauriello M, Passàli FM. Influence of Waldeyer’s ring hypertrophy on snoring and sleep Apnea. Adv Otorhinolaryngol. 2011;72:132–135.
- 2. Redline S, Amin R, Beebe D, et al. The childhood adenotonsillectomy trial (CHAT): rationale, design, and challenges of a randomized controlled trial evaluating a standard surgical procedure in a pediatric population. Sleep. 2011:34(11):1509–1517.
- 3. Yang SZ, Zhou CY, Wang ZL, et al. Preliminary experience of surgical treatment for torus tubarius hypertrophy in children. Chinese J Otorhinolaryngol Head Neck Surg. 2022;57(4):505–509.
- 4. Kim JW, Rhee CS, Jung HJ. Partial resection of hypertrophic torus tubarius for recurred snoring: case series. Medicine. 2020;99(10):e19329.
- 5. Honda K, Tanke M, Kumazawa T. Otitis media with effusion and tubal tonsil (video). Acta Otolaryngologica. 1988;105(Sup 454):218–221.
- 6. Monroy A, Behar P, Brodsky L. Revision adenoidectomy: a retrospective study. Int J Pediatr Otorhinolaryngol. 2008;72(5):565–570.
- 7. Merati AL, Rieder AA. Normal endoscopic anatomy of the pharynx and larynx. Am J Med. 2003;115(Suppl 3A):10S-4S.
- 8. Dogru M, Evcimik MF, Calim OF. Does adenoid hypertrophy affect disease severity in children with allergic rhinitis? Eur Arch Otorhinolaryngol. 2016;274:209–213.
- 9. Modrzynski M, Zawisza E. An analysis of the incidence of adenoid hypertrophy in allergic children. Int J Pediatr Otorhinolaryngol. 2007;71(5):713–719.
- 10. Fabio P, Mara DA, Alessandro P, et al. Adenoids and clinical symptoms: epidemiology of a cohort of 795 pediatric patients. Int J Pediatr Otorhinolaryngol. 2015;79(12):2137–2141.
- 11. Adegbiji WA, Olajide GT, Olajuyin AO, Aremu SK, Olusola AG. Pattern of allergic rhinitis among children in Ekiti, Nigeria. Int J Pediatr Otorhinolaryngol. 2018;106:75–79.
- 12. Wang F, Zhou C, Zhang J, Yan Q, Han Z, Dai Z. Correlation between allergic rhinitis and childhood obstructive sleep apnea-hypopnea syndrome. J Clin Otorhinolaryngol Head Neck Surg. 2012;26(6):260–262.
- 13. Tuhanıoğlu B, Erkan SO. Evaluation of the effects of montelukast, mometasone furoate, and combined therapy on adenoid size: a randomized, prospective, clinical trial with objective data. Turk J Med Sci. 2017;47:1736–1743.
- 14. Al-Mazrou KA, Al-Khattaf AS. Adherent biofilms in adenotonsillar diseases in children. Arch Otolaryngol Head Neck Surg. 2008;134(1):20–23.
- 15. Marple BF. Allergic rhinitis and inflammatory airway disease: interactions within the unified airspace. Am J Rhinol Allergy. 2010;24(4):249–254.
- 16. Modrzynski M, Zawisza E. An analysis of the incidence of adenoid hypertrophy in allergic children. Int J Pediatr Otorhinolaryngol. 2007;71(5):713–719.