Introduction
Rhinoplasty is an intricate procedure and is therefore one of the most challenging, frequently executed surgical aesthetic procedures of the face. It involves several diverse approaches according to the specific deformities. - Rhinoplasty involving osteotomy of the nasal bones is one of the riskiest processes and results in a less controllable outcome. Osteotomy is generally performed in cases of correction of open roof deformity, reduction in the nasal pyramid, removal of convexity or unevenness, and straightening of the nasal bones. Lateral, medial, transverse, intermediate, and oblique are various techniques performed in the osteotomy. The process is associated with various challenges and unpredictable complications such as bleeding, ecchymosis, and edema ; therefore, a rapid recovery is essential for patients to ensure a successful outcome. The duration of surgery, quality of surgery, and thickness of nasal skin are crucial factors which are usually associated with periorbital edema and ecchymosis. The root source of these impediments is soft tissue injuries. , The extent of edema and ecchymosis after rhinoplasty also depends upon other factors such as the presence of any coagulation disorders, undue subcutaneous fat, the type of surgical procedure carried out, the type of osteotomy, the location differences of the arteria angularis, and any drug use prior to surgery.
The application of a diverse range of surgical techniques also influences the postoperative edema and ecchymosis rates of rhinoplasty. Every modus operandi has unique advantages and disadvantages. A study by Kilic et al showed that endonasal surgery produced better results in terms of a reduction in postoperative edema and ecchymosis. Further, the results of a study carried out by Ilhan et al suggest that rhinoplasty with ultrasonic osteotomy is associated with lower rates of edema and ecchymosis in the early postoperative phase than with conventional osteotomy. The researchers set out that the primary limitations of conventional osteotomy are blind manipulation and insufficient surgical experience.
The majority of aesthetic surgeons focus solely on the operative procedures themselves, and skin thickness receives very little attention. It is reported by many surgeons that the typical Middle Eastern nose presents a very challenging rhinoplasty due to the presence of a bulky skin envelope, an overprojecting osseocartilaginous vault, weak alar cartilages with limited support, and petite middle and medial crura. Thus, this study was conducted to evaluate the relationship between nasal skin thickness and postoperative periorbital ecchymosis and edema among patients who underwent rhinoplasty at the King Abdulaziz University Hospital. This was a pioneer attempt by the author to evaluate nasal skin thickness as a predictor for rhinoplasty outcomes.
Material and Methods
A prospective study was conducted among all patients operated on for rhinoplasty at King Abdulaziz University Hospital, Department of Otolaryngology, Riyadh, Saudi Arabia, between May and December 2018. Ethical clearance obtained from the institutional review board of the King Abdulaziz University Hospital. All patients above the age of 18 years who underwent open-approach single lateral osteotomy were included in the study, excluding patients with chronic diseases (hypertension, diabetes mellitus, rheumatological diseases, abnormal hemostatic values or using anticoagulants medication, skin diseases), smokers, and those who could not complete their follow-ups resulting in missing data. After setting inclusion and exclusion criteria, the total sample size was 54 patients and informed consent was obtained from all patients before commencing the study.
To determine the relationship between nasal skin thickness and postoperative periorbital ecchymosis and edema among patients who underwent rhinoplasty surgery, mean nasal skin thickness was obtained by Obagi skin pinch test. It is a simple and reliable method in which thin, normal, and thick skin are evaluated for dermal thickness at a keystone junction, with averages of 0.3 mm (0.2-0.4 mm), 0.5 mm (0.3-1.1 mm), and 0.9 mm (0.6-1.2 mm), respectively.
Next, all patients were evaluated postoperatively by an assigned surgeon for periorbital edema and ecchymosis on the 1st, 3rd, 7th, and 21st days post-surgery by using a 4-grade scale developed by Gürlek et al. (Figure 1 and 2). Periorbital edema and ecchymosis scores ranged from phases 0 to 4, whereby phase 1 comprised minimal edema, phase 2 comprised open eyelids reaching the iris due to the effect of edema, phase 3 comprised open eyelids showing only the pupils due to the effect of edema, and phase 4 comprised eyelids completely closed due to generalized edema (Figure 1). Similarly, the periorbital ecchymosis scores were 0 (none), (+)1 (in the medial canthus), (+)2 (extending to the pupil), (+)3 (past the pupil), and (+)4 (extending to the lateral canthus) (Figure 2). Data collection included the following variables: demographic data (gender, age), mean nasal skin thickness, surgical factors (time of surgery, extent of intraoperative bleeding), and scoring for periorbital ecchymosis and edema.
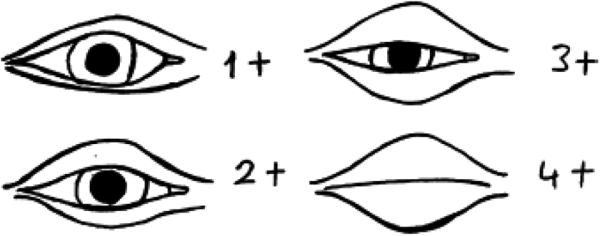
Figure 1
Scale for eyelid edema: 0 (none), (+1) (minimal), (+2) (covering to iris), (+3) (extending to the pupil), and (+4) (massive edema).
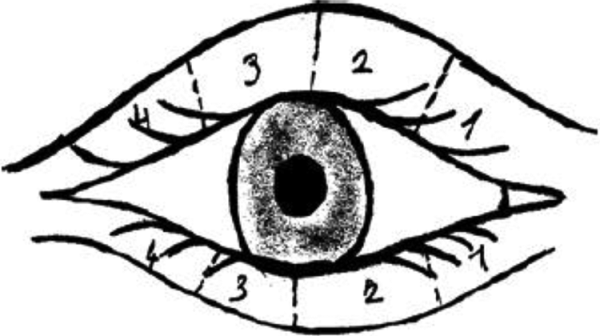
Figure 2
Scale for periorbital ecchymosis: 0 (none), (+1) (in the medial canthus), (+2) (extending to the pupil), (+3) (past the pupil), and (+4) (extending to the lateral canthus).
The statistical analysis was done by Statistical Package of Social Sciences (SPSS) version 20, mean and frequency were calculated for demographic details, and 1-way analysis of variance was used to compare the mean values of edema and ecchymosis with nasal skin thickness. A P value less than .05 is considered as significant.
Results
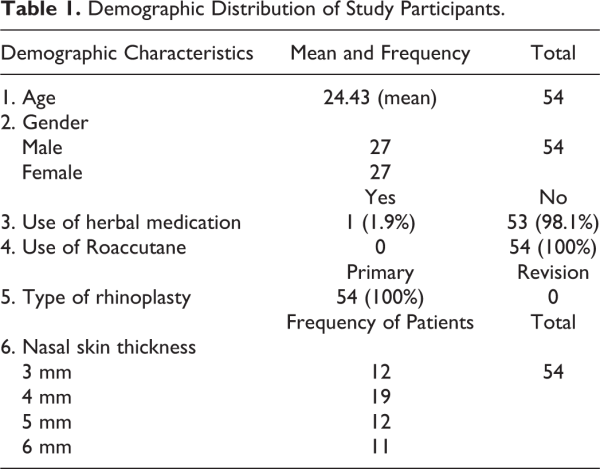
A total of 54 patients participated in this study with ages ranging from 19 to 33 years, and a mean age of 24.43, with equal gender distribution. In this study, only 1 patient used herbal medication and Roaccutane, whereas aspirin was not used by a single patient. Patients with any skin diseases were not included in the study; all patients who were included underwent primary rhinoplasty without revision. In terms of nasal thickness, the mode nasal thickness (19 patients) was 4 mm, followed by 3, 5, and 6 mm, present in 12, 12, and 11 patients, respectively. Demographic details of study participants are shown in Table 1.
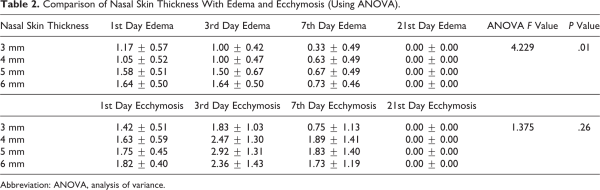
Comparison of nasal skin thickness with postoperative edema on the first, third, and seventh days showed that patients with thickened noses (6 mm) had the highest rates of edema with mean values of 1.64 ± 0.50, 1.64 ± 0.50, and 0.73 ± 0.46, correspondingly. Patients with 5, 4, and 3 mm nasal skin thickness generally experienced a less severe form of edema. The severity of edema was higher during the initial days (1st and 3rd) post-surgery, and after that was decreased. These results illustrated that the degree of edema was significantly associated with the thickness of the nose (P = .001). At the same time, in relation to the rates of ecchymosis, the first day examination presentation was higher in patients with 6 mm (1.82 ± 0.40) nasal skin thickness, but on the third and seventh day examinations, it was higher in 5 mm (2.92 ± 1.31) and 4 mm (1.89 ± 1.41) skin thickness, respectively. Both edema and ecchymosis were reduced on the 21st day examinations. This showed that the degree of ecchymosis was not significantly correlated with the thickness of the nose (P = .26). The comparison of nasal skin thickness with the degree of edema and ecchymosis is shown in Table 2.
Discussion
This was a prospective study among patients operated on for rhinoplasty conducted to determine the relationship between nasal skin thickness and postoperative periorbital ecchymosis and edema. The study looked at a total of 54 patients who participated in this study, with ages ranging from 19 to 33 years, with a mean age of 24.43 years. A similar study by Sriprakash et al analyzed patients with ages ranging from 18 to 45, with a mean age of 26. In our study, equal gender distribution was present, demonstrating that both genders’ rhinoplasty appeals to both men and women. A study by Ghamivi et al also had an equal gender distribution, whereas the study conducted by Sriprakash et al focused significantly more on males than females who had undergone rhinoplasty. In this study, only 1 patient used herbal medication and aspirin was not used by a single patient. Roaccutane was also used by only 1 patient, which may be significant when considering a study by Allen et al, who found that the use of isotretinoin was associated with nasal tip deformities after rhinoplasty. Patients with any skin diseases were not included in the study; all patients who were included underwent primary rhinoplasty without revision. In terms of nasal thickness, the mode nasal thickness (19 patients) was 4 mm, followed by 3, 5, and 6 mm, present in 12, 12, and 11 patients, respectively.
According to this study, postoperative edema and ecchymosis were connected with the thickness of nasal skin. This may be because greater nasal thickness interferes with lymphatic drainage and therefore results in increased rates of edema. Various researchers have determined that nasal bone thickness is also an essential factor that determines soft tissue damage during osteotomy, and soft tissue damage is directly related to edema and ecchymosis. In this study, the degree of edema and ecchymosis was higher in the initial postoperative days (1st and 3rd days) and after that it was reduced. This coincides with the results shown by Coroneos et al that the most severe presentations of edema and ecchymosis occur from postoperative days 1 to 3.
Patients with thick nasal skin can present challenges during rhinoplasty because thick nasal skin is loaded with sebaceous glands and subcutaneous tissue which can often obstruct achieving desirable results postoperatively. Thick nasal skin is associated with a failure of contraction, which may lead to excessive scar tissue formation and impaired lymphatic drainage, resulting in edema and ecchymosis. , Rhinoplasty is one of the most popular cosmetic surgical procedures worldwide, but it remains very difficult to obtain the desired results after rhinoplasty in patients with thick nasal skin. Correct pre- and postsurgical management depends upon the type of nasal skin. , The typical noses of Middle Easterns present challenges in rhinoplasty because of the presence of profound, thick skin envelopes and an overprojecting nose. This study provides additional guidance to select suitable cases for rhinoplasty and to manage further postoperative complications including edema and ecchymosis. The results of this study are derived from a single center with specific surgical techniques, and the sample size of this study was small, which could be considered limitations of this study. Further, in this study, we did not compare the degree of edema and ecchymosis in males and females; we only assessed the correlation between nasal skin thickness and postoperative edema and ecchymosis without considering gender.
Conclusion
This study concludes that the severity of edema and ecchymosis correlates with nasal skin thickness. The degree of edema and ecchymosis was higher during the initial postoperative examinations, but following that it was reduced and completely diminished by the 21st day of post-surgery.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
Badi Aldosari
https://orcid.org/0000-0001-9865-3795
References
- 1. Al Arfaj AM. The use of nasal packing post rhinoplasty: does it increase periorbital ecchymosis? A prospective study. J Otolaryngol Head Neck Surg. 2015;44(1):22.
- 2. Alharethy S, Aldrees T, Aljrid R, Alanazi A, Algaryan SK, Jang YJ. Common nasal deformities among rhinoplasty patients in a university hospital in Saudi Arabia. Ann Saudi Med. 2017;37(3):207–211.
- 3. Ilhan AE, Cengiz B, Caypinar Eser B. Double-blind comparison of ultrasonic and conventional osteotomy in terms of early postoperative edema and ecchymosis. Aesthet Surg J. 2016;36(4):390–401.
- 4. Caglar E, Celebi S, Topak M, Develioglu NO, Yalcin E, Kulekci M. How can periorbital oedema and ecchymose be reduced in rhinoplasty? Eur Arch Otorhinolaryngol. 2016;273(9):2549–2554.
- 5. Manafi A, Babaki AE, Mehrabani G, Shahlaee A, Manafi A. Can we add auricular composite graft to our rhinoplasty armamentarium? World J Plast Surg. 2013;2(1):33–40.
- 6. Sakallioglu Ö, Cingi C, Polat C, Soylu E, Akyigit A, Soken H. Open versus closed septorhinoplasty approaches for postoperative edema and ecchymosis. J Craniofac Surg. 2015;26(4):1334–1337.
- 7. Sari E, Simsek G. Comparison of the effects of total nasal block and central facial block on acute postoperative pain, edema, and ecchymosis after septorhinoplasty. Aesthet Plast Surg. 2015;39(6):877–880.
- 8. Kiliç C, Tuncel Ü, Cömert E, Sencan Z. Effect of the rhinoplasty technique and lateral osteotomy on periorbital edema and ecchymosis. J Craniofac Surg. 2015;26(5):e430–e433.
- 9. Taşkın Ü, Batmaz T, Erdil M, Aydın S, Yücebaş K. The comparison of edema and ecchymosis after piezoelectric and conventional osteotomy in rhinoplasty. Eur Arch Otorhinolaryngol. 2017;274(2):861–865.
- 10. Obagi ZE. The Art of Skin Health Restoration and Rejuvenation. 2nd ed. London, United Kingdom: CRC Press; 2014.
- 11. Gurlek A, Fariz A, Aydogan H, Ersoz-Ozturk A, Eren AT. Effects of different corticosteroids on edema and ecchymosis in open rhinoplasty. Aesthetic plastic surgery. 2006;30(2):150–154.
- 12. Sriprakash V. Efficacy of the intraoperative cold saline-soaked gauze compression on intraoperative bleeding, postoperative oedema and ecchymosis in rhinoplasty. IJCMR. 2017;4(3):707–710.
- 13. Ghavimi MA, Nezafati S, Yazdani J, et al. Comparison of edema and ecchymosis in rhinoplasty candidates after lateral nasal osteotomy using piezosurgery and external osteotomy. Journal of advanced pharmaceutical technology & research. 2018;9(3):73.
- 14. Allen BC, Rhee JS. Complications associated with isotretinoin use after rhinoplasty. Aesthet Plast Surg. 2005;29(2):102–106.
- 15. Ortiz-Monasterio F, Lopez-Mas J, Araico J. Rhinoplasty in the thick-skinned nose. Br J Plast Surg. 1974;27(1):19–24.
- 16. Kuran I, Özcan H, Usta A, Bas L. Comparison of four different types of osteotomes for lateral osteotomy: a cadaver study. Aesthet Plast Surg. 1996;20(4):323–326.
- 17. Coroneos CJ, Voineskos SH, Cook DJ, Farrokhyar F, Thoma A. Perioperative corticosteroids reduce short-term edema and ecchymosis in rhinoplasty: a meta-analysis. Aesthetic surgery journal. 2016;36(2):136–146.
- 18. Özkul MH, Kocagöz DG, Balıkcı HH, Verim A, Yaşar H. A practical method for assessing nasal skin quality. European Archives of Oto-Rhino-Laryngology. 2013;270(6):1839–1842.
- 19. Cobo R, Camacho JG, Orrego J. Integrated management of the thick-skinned rhinoplasty patient. Facial Plast Surg. 2018;34(01):003–008.