The chemical properties of clindamycin can contribute to clindamycin-induced mucosal injury of the larynx, pharynx, and gastrointestinal tract. Esophagitis and laryngitis after consumption of clindamycin are rare. We present a 66-year-old male who experienced laryngo-esophagitis after swallowing clindamycin following a dental procedure.
A 66-year-old never-smoker Caucasian male presented with initial symptoms of intense throat pain after swallowing a 300-mg clindamycin pill. The patient had no previously reported allergic reaction to clindamycin. He did have previously reported swelling reactions to penicillin and nonsteroidal anti-inflammatory drugs. He complained of acute onset of throat pain with the sensation that the clindamycin was stuck in his throat. He described cycles of retching and drinking water for about an hour, and he denied vomiting and shortness of breath. During one episode, the patient reported coughing up a small amount of phlegm containing bits of the clindamycin capsule. Upon arrival to the emergency department, he complained of constant odynophagia and hoarseness. Ranitidine was prescribed for the patient’s reflux-like symptoms. An esophagogastroduodenoscopy performed the following day reported severe unilateral congestion and ulceration of the aryepiglottic fold and other structures in the posterior oropharynx as well as congested erythematous and eroded mucosa in the gastric body, incisura, and antrum. The esophagus and duodenum were reported to be normal. Biopsies from the gastric body, incisura, and antrum showed gastric mucosa with reactive gastropathy without Helicobacter pylori-like microorganisms or dysplasia. An otolaryngology consultation was obtained the same day for constant pain as well as subsequent hoarseness and odynophagia limiting his eating. Laryngoscopy showed erythema and edema of both arytenoids and interarytenoid mucosa as well as erythema and edema of both vocal folds (Figure 1). There was symmetric vocal fold movement. Thick, yellow endolaryngeal secretions with pooling in the hypopharynx was present, as well as edema of the epiglottis with erythema (Figure 2). The final impression was clindamycin-induced esophagitis and laryngitis. A prednisone taper and lidocaine gargle for inflammation and pain alleviation were prescribed. Omeprazole was added to the patient’s current medications for the retrograde esophageal secretions. Upon follow-up 2 months later, laryngoscopy revealed significantly decreased erythema and edema. The findings from endoscopy suggested that the clindamycin tablet caused a chemical burn of the esophageal and laryngeal mucosa.
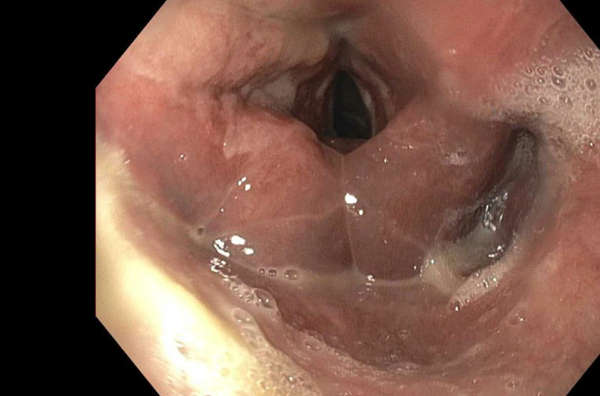
Figure 1
Laryngoscopic view demonstrating arytenoid edema and laryngeal inflammation.
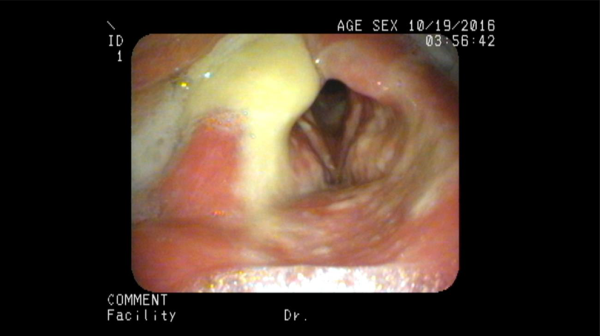
Figure 2
Thick endolaryngeal secretions with pooling in the hypopharynx.
The occurrence of esophagitis and esophageal ulcers is a well-known adverse reaction to pill ingestion, which has been described in detail. Antibiotics including doxycycline, tetracycline, and clindamycin are the leading causative agents of drug-induced esophagitis. Inflammation and ulcers in the esophagus have been listed as rare side effects of clindamycin on WebMD. In contrast, laryngitis and laryngotracheitis are not described as possible adverse effects in the product information of clindamycin, and reports are lacking in the medical literature. Therefore, drug-induced esophagitis and laryngitis are uncommon together.
A major contributing etiology to laryngitis is a history of gastroesophageal reflux disease, but the reported patient did not present with such a history. However, the more commonly seen drug-induced esophagitis has been attributed to a lack of education on pill ingestion. It is advised that patients take medications with at least 4 ounces of water and in the upright position, waiting at least 10 minutes before lying down.
Most cases of drug-induced esophagitis, those caused by medications with low acid pH that can create localized ulcers, resolve on their own once the causative drug is discontinued. It is important to avoid reinjury with the drug. Clinicians who treat patients with swallowing dysfunctions should especially be aware of this hazard.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
Amy L. Rutt
https://orcid.org/0000-0002-7704-6328
References
- 1. Jaspersen D. Drug-induced oesophageal disorders. Drug Safety. 2000;22(3):237–249.
- 2. Kikendall JW. Pill esophagitis. J Clin Gastroenterol. 1999;28(4):298–305.
- 3. Zografos GN, Georgiadou D, Thomas D, Kaltsas G, Digalakis M. Drug-induced esophagitis. Dis Esophagus. 2009;22(8):633–637.
