Introduction
Tonsillectomy is a universal surgical operation. The indications for a tonsillectomy include recurrent tonsillitis, obstructive sleep apnea, and recurrent peritonsillar abscess.- In the pediatric population, the most widely recognized indications for a tonsillectomy are recurrent tonsillar infections and bilateral tonsillar hypertrophy with disturbed sleep. Although tonsillectomies are generally safe operations unlikely to be associated with complications, post-tonsillectomy hemorrhage is a major complication. Post-tonsillectomy hemorrhage within the first 24 hours postoperative is known as primary post-tonsillectomy hemorrhage, while bleeding after 24 hours postoperative—typically following discharge—is known as secondary post-tonsillectomy hemorrhage. A revisit to the operating room for surgical control of the hemorrhage maybe required for severe or uncontrolled post-tonsillectomy hemorrhage., Primary bleeding has been linked to multiple factors, such as operative technique, inadequate contraction of the blood vessels in the tonsillar bed, and deficient coagulation. Secondary bleeding is reported to be associated to many factors, such as sex, age, use of nonsteroidal anti-inflammatory drug (NSAIDs) medications, poor oral intake post-tonsillectomy, and seasonal variations.,,
Several studies have investigated possible risk factors contributing in post-tonsillectomy hemorrhage. One recently conducted study in Australia evaluated multiple risk factors that predicted post-tonsillectomy bleeding. It was revealed that patients taking ibuprofen were at risk of post-tonsillectomy bleeding. Additionally, the risk of post-tonsillectomy bleeding increased with each year of age. Similarly, another study unconcealed that the surgeon’s level of expertise was additionally considerable related to post-tonsillectomy bleeding. Tonsillectomies performed by trainee-level surgeons had more risk of post-tonsillectomy bleeding compared to senior consultants. One study compared the techniques of tonsillectomy and found that the risk of post-tonsillectomy hemorrhage was higher in patients undergoing bipolar diathermy compared to the cold dissection technique.
In Saudi Arabia, childhood obesity has a higher prevalence compared to other countries., Therefore, it’s vital to check whether obesity is a contributing factor for post-tonsillectomy hemorrhage among our population. Additionally, countries weather variations may have a possible influence on post tonsillectomy bleeding rate, as has been suggested in previous studies. Harounian et al suggested that the need for and use of tonsillectomy may vary by geography and sociodemographic characteristics.
Post-tonsillectomy hemorrhage is a major concern to surgeons and patients, but the published data on risk factors contributing to secondary post-tonsillectomy hemorrhage in Saudi Arabia are limited. This study aims to discover the variables correlated with post-tonsillectomy hemorrhage in Saudi Arabia.
Materials and Methodology
This retrospective chart review study was directed at King Abdullah Specialized Children’s Hospital, Riyadh, Saudi Arabia. It focuses on the outcome of pediatric patients under the age of 14 years who underwent elective tonsillectomy from December 2015 to December 2017. Patient data collection variables included demographic data, body mass index (BMI), presence of comorbidities, syndromes, history, number of documented recurrent tonsillitis attacks (in light of presence of sore throat and one or more of the following: temperature 38.3 °C [101°F], cervical adenopathy, tonsillar exudate, or positive test for group A β-hemolytic streptococcus), and history of sleep breathing disorder/obstructive sleep apnea. Surgery data included date of surgery, date of discharge after tonsillectomy, surgeon’s expertise level (senior [registrar and above] vs junior), concurrent adenoidectomy tonsillectomy procedure, dissection technique (monopolar, bipolar, or cold dissection), physician documentation of secondary tonsillectomy bleeding, date of bleeding, medication use post-tonsillectomy (including ibuprofen or other NSAIDs, paracetamol, and antibiotics), intraoperative use of local anesthesia (using lidocaine only), and the season when the surgery was performed. The season was categorized as the cold season (November to February) and warm season (March to October).
Statistical Analysis
The cohort description is reported in frequencies and percentages. To determine the significant association between the variables, the logistic regression was fitted as a univariable model for single associations with all variables. Then, a multivariable model was created. Differences were considered significant with a P value less than .05.
Results
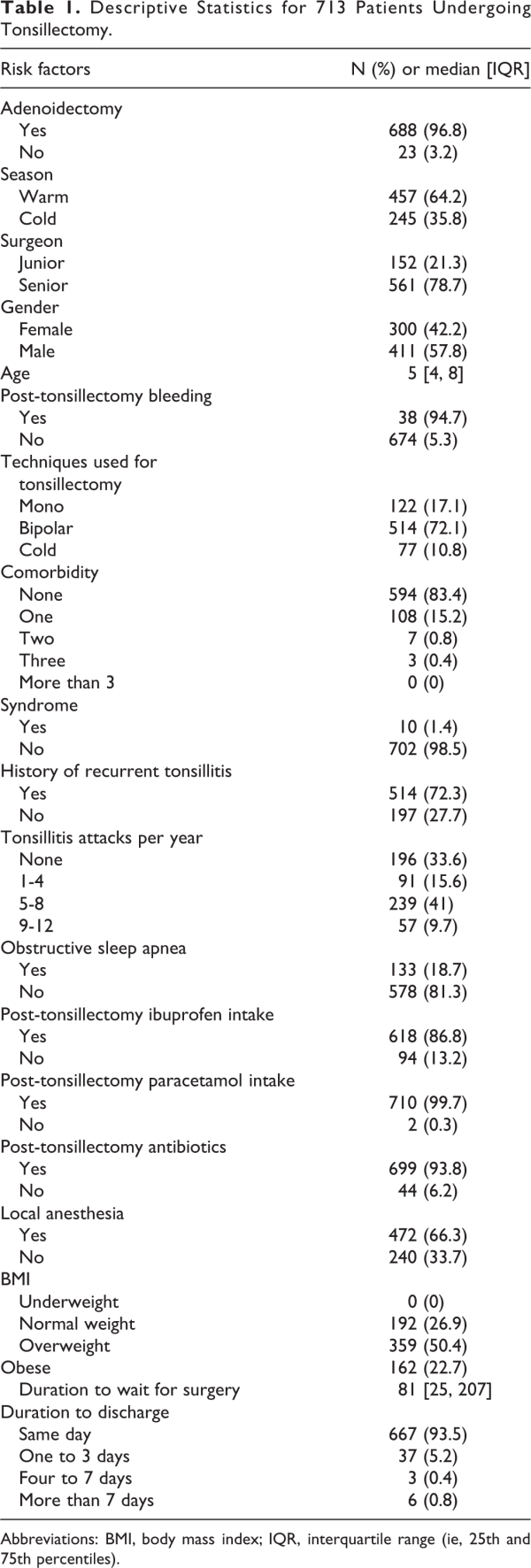
The present study evaluated the risk factors of post-tonsillectomy bleeding among 713 children who underwent tonsillectomies. Table 1 shows the general descriptive characteristics of the group by risk factors. The median age of the study population was 5 years (interquartile range: 4-8; range: 1-13). Male patients accounted for 57.6% of the study population.
Regarding patient history, 72.1% of patients had a history of recurrent tonsillitis, and 33.5% experienced 5 to 8 attacks per year. Sleep disorder breathing/obstructive sleep apnea was reported in 18.7% of patients. The BMI measures of all patients revealed that 50.4% were overweight (BMI between 85th and 95th percentile), and only 26.9% had a normal weight (BMI between 5th and 85th percentile). These percentile categorizations for BMI in children were adopted from expert committee recommendation. In the sample, 96.5% had adenoidectomy, and 64.1% of these proceedings were performed in the warm season. A total of 78.7% of tonsillectomies were carried out by senior surgeons. Post-tonsillectomy bleeding occurred in 5.3% of these tonsillectomies. The surgeons used the bipolar tonsillectomy approach in 72.1% cases. There were no comorbidities in 83.3% of the participants, and 98.5% were also free of any syndrome.
The majority of patients took ibuprofen (86.7%), paracetamol (99.6%), and antibiotics (93.8%) post-tonsillectomy. Local anesthesia was given in 66.2% of patients. There was a median waiting period of 81 days for surgery after initial appointment (interquartile range: 25-207; range: 1-803). The majority of patients (93.5%) were discharged on the same day, and 5.2% were discharged within 1 to 3 days due present of sleep disorder breathing or other comorbidities such as bronchial asthma.
The majority of post-tonsillectomy bleeding was reported in the month of December, but this was not statistically significant (P = .8). The frequency bar chart of number of cases reported by month is presented Figure 1.
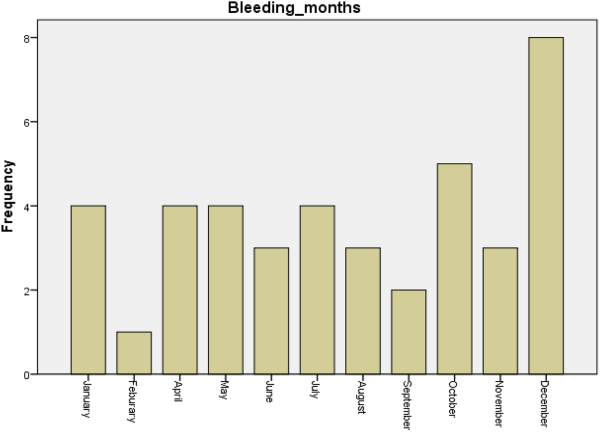
Figure
1. Secondary post tonsillectomy bleeding across the months.
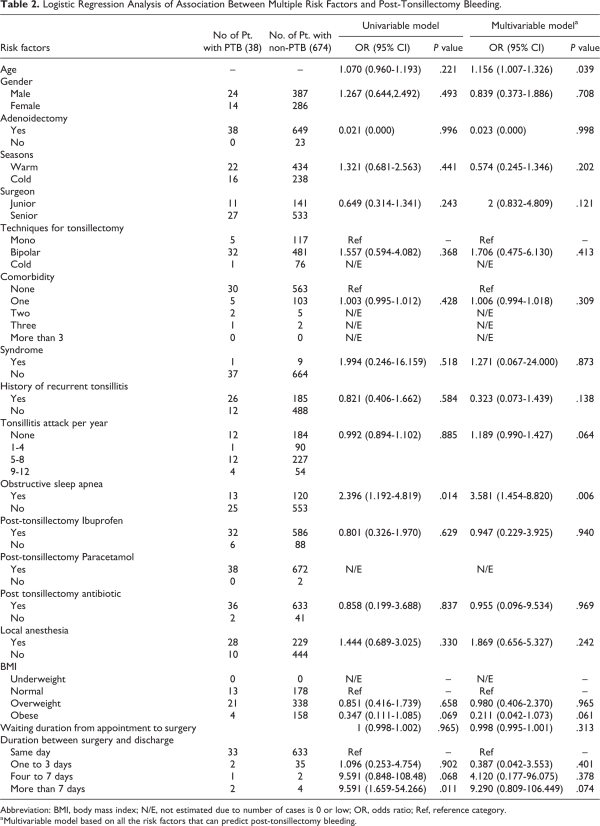
Table 2 shows the findings from the logistic regression analysis using univariable and multivariable models to determine the effects of multiple risk factors on the potential likelihood of post-tonsillectomy bleeding. The logistic regression (multivariable model), which classified 95.3% of cases, revealed 19.2% (Nagelkerke R2) variance in post-tonsillectomy bleeding. The results revealed that for increasing age (up to 13 years of age), there was an increase in the risk of post-tonsillectomy bleeding (odds ratio [OR] = 1.156; 95% CI = 1.007-1.326; P = .039). Likewise, a similar increase in odds of post-tonsillectomy bleeding was observed in both the univariable analysis (OR = 2.396; 95% CI = 1.192-4.819; P = .014) and multivariable analysis (OR = 3.581; 95% CI = 1.454-8.820; P = .006) for sleep disorder breathing/obstructive sleep apnea. In the univariable analysis, it was found that the longer the duration between surgery and discharge, the greater the odds of post-tonsillectomy bleeding (OR = 9.591; 95% CI = 1.659-54.266; P = .011), but this was no longer significant in the multivariable analysis (OR = 9.290; 95% CI = 0.809-106.449; P = .074).
Discussion
In otolaryngology, malpractice in tonsillectomy has been associated with an increase in morbidity and mortality. Hemorrhage in post-tonsillectomy can be life threatening. Some of the potential risk factors associated with post-tonsillectomy hemorrhage and hospital admission include surgical technique, surgeon’s skill level, sex and age of the patient, BMI, and indication for tonsillectomy.,, However, in the present study, age and obstructive sleep apnea were found to be statistically significant risk factors for post-tonsillectomy bleeding.
In the present study, 96.5% of patients had adenoidectomy. When evaluated through a multivariate model, this was not found to have a statistically significant impact on post-tonsillectomy bleeding (P = .998). These findings are similar to previous study that suggested addition adenoidectomy (adenotonsillectomy) did not increase the chance of post-tonsillectomy bleeding. Studies have reported that postoperative bleeding in tonsillectomy patients after adenotonsillectomy leads to increased length of hospital stay, higher rate of readmissions, and greater financial burden., The present study found no statistically significant association between season and the risk of post-tonsillectomy bleeding, similar to a previous study.
A statistically significant association was found between age and post-tonsillectomy bleeding (OR = 1.151; 95% CI = 1.007-1.326; P = .039). Previous studies have shown that age was found to be a major predictor of post-tonsillectomy hemorrhage.,, In contrary, Ordemann et al found that child age did not increase the risk of post-tonsillectomy hemorrhage. Spektor et al found that children older than 11 years were more prone to post-tonsillectomy hemorrhage. The theoretical underpinning of age-associated bleeding is the longer duration of tonsillitis in older patients. According to Tomkinson et al, the risk of post-tonsillectomy hemorrhage increased significantly in patients older than 12 years. Aljabr et al also reported age as a major predictor of post-tonsillectomy hemorrhage.
In the current study, sex was found to be statistically nonsignificant in determining post-tonsillectomy hemorrhage (OR = 0.839; 95% CI = 0.373-1.886; P = .708). In contrast, one previous study revealed that the risk of post-tonsillectomy bleeding was found to be lower in females compared to males. However, a recently conducted study reported that the risk of post-tonsillectomy hemorrhage is similar in both sexes.
The current study also revealed no significant association between tonsillectomy technique and post-tonsillectomy bleeding. These findings are consistent with the results of the study by Kwok et al who found no significant difference in hemorrhage between cold dissection and bipolar diathermy tonsillectomy. In contrast, a different study reported that bipolar diathermy leads to patients being vulnerable to delayed hemorrhage. Furthermore, bipolar diathermy was also associated with increased postoperative pain. Alternatively, the proponents of the bipolar surgical procedure claim that it is a more efficient and faster procedure compared to cold dissection. Sarny et al found that the bipolar or coblation method enhanced the risk of postoperative hemorrhage compared to cold steel tonsillectomy.
Several authors have reported that the risk of post-tonsillectomy bleeding depends on the skill level of the surgeon, with the risk of bleeding increasing when procedures are performed by trainees., In the current study, there was no association between the surgeon’s skill level and post-tonsillectomy bleeding which in keeping with other previous studies., However, a surgeon’s inexperience and dissection in the wrong plane results in more post-tonsillectomy bleeding. Furthermore, the operation time is increased, leading to a greater loss of blood.
In present study, post-tonsillectomy bleeding was not found to be significant correlated with comorbidity, syndrome, or the history of recurrent tonsillitis which in line with other previous study. No previous studies have found an impact of syndromes on postoperative bleeding. However, the history of recurrent tonsillitis has been found to be significantly associated with post-tonsillectomy bleeding, with the incidence of post-tonsillectomy bleeding higher in cases of recurrent infections.,
Literature has shown that sleep-related obstructive apnea is a predictor of Post-tonsillectomy bleeding., The current findings revealed a statistically significant association between obstructive sleep apnea and post-tonsillectomy bleeding in both the univariable (OR = 2.396; 95% CI = 1.192-4.819; P = .014) and multivariable (OR = 3.581; 95% CI = 1.454-8.820; P = .006) analyses. The current study revealed no impact of medication intake, included ibuprofen, paracetamol, and antibiotics, on post-tonsillectomy bleeding. However, there have been questions over the use of ibuprofen and other NSAIDs in post-tonsillectomy patients. While recent studies failed to find an association between NSAIDs and post-tonsillectomy bleeding, 2 studies reported that the administration of ibuprofen increases hemorrhage in the postoperative phase.,
In regard with the use of antibiotic, our findings were in consistent with a recent, meta-analysis which showed that, the use of antibiotic did not reduce the incidence post-tonsillectomy bleeding. Moreover, the use of antibiotics in tonsillectomy patients does not comply with the recommended protocols of antibiotics usage.
Local anesthesia was also found to be a statistically non-significant risk factor for post-tonsillectomy bleeding. In a previous study, the administration of lidocaine and epinephrine was found to be associated with post-tonsillectomy bleeding in 12.5% of patients. The researchers explained that the bleeding rate was less when only lidocaine was administered. This suggests that the administration of epinephrine along with lidocaine increases bleeding rates and excluding epinephrine should facilitate accurate hemostasis.
The majority of patients in the current study were overweight yet this was not surprising in light of the fact that various studies have demonstrated high obesity/overweight prevalence among children in Saudi Arabia., The current findings demonstrated that BMI had a non-significant impact on postoperative bleeding for both the univariable (OR = 0.851; 95% CI = 0.416-1.739; P = .658) and multivariable (OR = 0.980; 95% CI = 0.406-2.370; P = .965) analyses. This coincides with the findings by Riechelmann et al and Spektor et al. In contrast, a previous study revealed that a BMI z-score of more than 2 was a risk factor in post-tonsillectomy patients. There is limited empirical evidence regarding the association between BMI and post-tonsillectomy bleeding. Childhood obesity is linked with a longer duration of anesthesia, prolonged operative time, and a greater rate of readmission after adenotonsillectomy. A recently conducted study argued that the risk of post-tonsillectomy bleeding was increased by 2.3 times in obese children. Why obesity increases the risk of bleeding is unclear. Burckardt et al reported that obesity is pro-inflammatory, and obese children are more likely to develop other comorbidities, such as fatty liver diseases, hyperlipidemia, and diabetes mellitus. These comorbidities put obese children at a greater risk of post-tonsillectomy hemorrhage.
The findings of the current study also revealed that the longer the duration before discharge post-surgery, the higher the odds were for post-tonsillectomy bleeding. In the univariable analysis, the odds of post-tonsillectomy bleeding in patients discharged after more than 7 days were found to be greater (OR = 9.591; 95% CI = 1.659-54.266; P = .011). These findings demonstrate that delayed discharge is one of the factors that can enhance the potential of post-tonsillectomy bleeding. However, most of the causes of delay discharge is poor oral intake which is maybe one of contribution factors for post tonsillectomy bleeding.
The primary limitation of this study was the lack of diverse data. The study was conducted in only 1 center, and thus there is a chance that cases of post-tonsillectomy bleeding were taken to other centers instead of returning to the initial surgery hospital. The findings could better represent large cohorts if multiple centers were added to the study. However, one of the strength of this study was that it was the first cohort study on the issue of post-tonsillectomy bleeding in the region. Therefore, the findings of this study may serve as a baseline for further investigation into the issue of post-tonsillectomy bleeding.
Conclusion
There are numerous risk factors associated with post-tonsillectomy bleeding. The factors evaluated in the current study revealed that age, obstructive sleep apnea, and longer hospital stay after tonsillectomy are significant risk factors for post-tonsillectomy bleeding. Previous literature revealed that the surgeon’s experience, surgical technique, medication usage, patient sex, and anesthesia influenced post-tonsillectomy bleeding. However, none of these factors was found to significantly increase the risk of post-tonsillectomy bleeding in our study. Furthermore, despite the patients using different medications, such as ibuprofen, paracetamol, and antibiotics, they did not show any related increase in the risk of post-tonsillectomy bleeding. The findings of the current study have contrasting results, and there is a need to perform a cross-sectional study to evaluate risk factors in multiple cohorts. In this way, a framework can be formulated to safely perform tonsillectomy and reduce the risk of morbidities and mortalities associated with post-tonsillectomy hemorrhage.
Acknowledgments
The authors are grateful for the support by the Deanship of Scientific Research at Prince Sattam Bin Abdulaziz, University, Al Kharj, Saudi Arabia.
Authors’ Note This research was approved by King Abdullah International Medical Research Center’s (KAIMRC), project number RC20/097/R. Turki Aldrees is now affiliated with Department of Otaloryngology-Head and Neck Surgery, Prince Sattam Bin Abdulaziz University, Al Khraj, Saudi Arabia.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
Turki Aldrees
https://orcid.org/0000-0001-5284-3956
References
- 1. Burton MJ, Glasziou PP, Chong LY, Venekamp RP. Tonsillectomy or adenotonsillectomy versus non-surgical treatment for chronic/recurrent acute tonsillitis. Cochrane Database Syst Rev. 2014;2014(11):CD001802.
- 2. Burton MJ, Goldstein NA, Rosenfeld RM. Cochrane Corner: extracts from the Cochrane Library: tonsillectomy or adenotonsillectomy versus non-surgical management for obstructive sleep-disordered breathing in children. Otolaryngol Neck Surg. 2016;154(4):581–585.
- 3. MacFarlane PL, Nasser S, Coman WB, Kiss G, Harris PK, Carney AS. Tonsillectomy in Australia: an audit of surgical technique and postoperative care. Otolaryngol Neck Surg. 2008;139(1):109–114.
- 4. Archer S, Rosenfeld R, Mitchell R, Baugh R. Clinical practice guideline: tonsillectomy in children. Otolaryngol Neck Surg. 2010;143:P12.
- 5. Chadha NK. Tonsillectomy return-to-theatre rates demonstrate a monthly and seasonal variation: an analysis of 256 799 patients. J Laryngol Otol. 2007;121:1088–1093.
- 6. Windfuhr JP, Chen YS, Remmert S. Hemorrhage following tonsillectomy and adenoidectomy in 15,218 patients. Otolaryngol Neck Surg. 2005;132(2):281–286.
- 7. Maksimović Z, Vranješ Ž, Stakić A, Zubčić Ž, Birtić D. Incidence of post-tonsillectomy and post-adenotonsillectomy hemorrhage in 5125 patients operated during the 1994-2005 period at department of Ent, head and neck surgery, Osijek University Hospital in Osijek, Croatia. Acta Clin Croat. 2007;46(3):247–250.
- 8. Eski E, Dogan I, Yilmaz I. Seasonal variation of secondary post tonsillectomy hemorrhage rates. B-ENT. 2011;7(3):165.
- 9. Kwok MM, Subramaniyan M, Rimmer J, Karahalios A. Post-tonsillectomy haemorrhage in Australia—a multivariable analysis of risk factors. Aust J Otolaryngol. 2018;1(1): 2.
- 10. Manimaran V, Mohanty S, Jayagandhi SK, Umamaheshwaran P, Jeyabalakrishnan S. A retrospective analysis of peroperative risk factors associated with posttonsillectomy reactionary hemorrhage in a teaching hospital. Int Arch Otorhinolaryngol. 2019;23(4):e403–e407.
- 11. Aljabr IK, Hassan FM, Alyahya KA. Post-tonsillectomy hemorrhage after bipolar diathermy vs. cold dissection surgical techniques in Alahsa region, Saudi Arabia. Alexandria J Med. 2016;52(2):169–172.
- 12. El Mouzan MI, Foster PJ, Al Herbish AS, et al. Prevalence of overweight and obesity in Saudi children and adolescents. Ann Saudi Med. 2010;30(3):203–208.
- 13. Al Dossary SS, Sarkis PE, Hassan A, Ezz El Regal M, Fouda AE. Obesity in Saudi children: a dangerous reality. East Mediterr Health J. 2010;16(9):1003–1008.
- 14. Harounian JA, Schaefer E, Schubart J, Carr MM. Pediatric adenotonsillectomy and postoperative hemorrhage: Demographic and geographic variation in the US. Int J Pediatr Otorhinolaryngol. 2016;87:50–54.
- 15. Barlow SE; Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–S192.
- 16. Kim MK, Lee JW, Kim MG, Ha SY, Lee JS, Yeo SG. Analysis of prognostic factors for postoperative bleeding after tonsillectomy. Eur Arch Oto-Rhino-Laryngology. 2012;269(3):977–981.
- 17. Perkins JN, Liang C, Gao D, Shultz L, Friedman NR. Risk of post-tonsillectomy hemorrhage by clinical diagnosis. Laryngoscope. 2012;122(10):2311–2315.
- 18. Nafiu OO, Green GE, Walton S, Morris M, Reddy S, Tremper KK. Obesity and risk of peri-operative complications in children presenting for adenotonsillectomy. Int J Pediatr Otorhinolaryngol. 2009;73(1):89–95.
- 19. Riechelmann H, Blassnigg EC, Profanter C, Greier K, Kral F, Bender B. No association between obesity and post-tonsillectomy haemorrhage. J Laryngol Otol. 2014;128(5):463–467.
- 20. Goldman JL, Ziegler C, Burckardt EM. Otolaryngology practice patterns in pediatric tonsillectomy: the impact of the codeine boxed warning. Laryngoscope. 2018;128(1):264–268.
- 21. Østvoll E, Sunnergren O, Ericsson E, Hemlin C, Hultcrantz E, Odhagen E, Stalfors J. Mortality after tonsil surgery, a population study, covering eight years and 82,527 operations in Sweden. Eur Arch Oto-Rhino-Laryngology. 2015;272(3):737–743.
- 22. Cadd B, Rogers M, Patel H, Crossland G. (Ton) silly seasons? Do atmospheric conditions actually affect post-tonsillectomy secondary haemorrhage rates? J Laryngol Otol. 2015;129(7):702–705.
- 23. Hussain S, O’Connell Ferster AP, Carr MM. Time between first and second posttonsillectomy bleeds. Int J Otolaryngol. 2017;2017:3275683.
- 24. Ordemann AG, Hartzog AJ, Seals SR, Spankovich C, Stringer SP. Is weight a predictive risk factor of postoperative tonsillectomy bleed? Laryngoscope Investig Otolaryngol. 2018;3(3):238–243.
- 25. Spektor Z, Saint-Victor S, Kay DJ, Mandell DL. Risk factors for pediatric post-tonsillectomy hemorrhage. Int J Pediatr Otorhinolaryngol. 2016;84:151–155.
- 26. Tomkinson A, Harrison W, Owens D, Harris S, McClure V, Temple M. Risk factors for postoperative hemorrhage following tonsillectomy. Laryngoscope. 2011;121(2):279–288.
- 27. Bhattacharyya N, Shapiro NL. Associations between socioeconomic status and race with complications after tonsillectomy in children. Otolaryngol Neck Surg. 2014;151(6):1055–1060.
- 28. Kshirsagar R, Mahboubi H, Moriyama D, Ajose-Popoola O, Pham NS, Ahuja GS. Increased immediate postoperative hemorrhage in older and obese children after outpatient tonsillectomy. Int J Pediatr Otorhinolaryngol. 2016;84:119–123.
- 29. Mofatteh MR, Salehi F, Hosseini M, Hassanzadeh-Taheri M, Sharifzadeh G, Hassanzadeh-Taheri M. Comparison of postoperative morbidity between conventional cold dissection and bipolar electrocautery tonsillectomy: which technique is better?. Braz J Otorhinolaryngol. 2019;753:1–7
- 30. Sarny S, Ossimitz G, Habermann W, Stammberger H. Hemorrhage following tonsil surgery: a multicenter prospective study. Laryngoscope. 2011;121(12):2553–2560.
- 31. Harju T, Numminen J. Risk factors for secondary post-tonsillectomy haemorrhage following tonsillectomy with bipolar scissors: four-year retrospective cohort study. J Laryngol Otol. 2017;131(2):155–161.
- 32. Burckardt E, Rebholz W, Allen S, Cash E, Goldman J. Predictors for hemorrhage following pediatric adenotonsillectomy. Int J Pediatr Otorhinolaryngol. 2019;117:143–147.
- 33. Reckley LK, Fernandez-Salvador C, Camacho M. The effect of tonsillectomy on obstructive sleep apnea: an overview of systematic reviews. Nat Sci Sleep. 2018;10:105.
- 34. McKeon M, Kirsh E, Kawai K, Roberson D, Watters K. Risk factors for multiple hemorrhages following tonsil surgery in children. Laryngoscope. 2019;129(12):2765–2770.
- 35. Lewis SR, Nicholson A, Cardwell ME, Siviter G, Smith AF. Nonsteroidal anti-inflammatory drugs and perioperative bleeding in paediatric tonsillectomy. Cochrane Database Syst Rev. 2013;2013(7):CD003591.
- 36. D’Souza JN, Schmidt RJ, Xie L, Adelman JP, Nardone HC. Postoperative nonsteroidal anti-inflammatory drugs and risk of bleeding in pediatric intracapsular tonsillectomy. Int J Pediatr Otorhinolaryngol. 2015;79(9):1472–1476.
- 37. Swanson RT, Schubart JR, Carr MM. Association of ibuprofen use with post-tonsillectomy bleeding in older children. Am J Otolaryngol. 2018;39(5):618–622.
- 38. Abdelhamid AO, Sobhy TS, El-Mehairy HM, Hamid O. Role of antibiotics in post-tonsillectomy morbidities; A systematic review. Int J Pediatr Otorhinolaryngol. 2019;118:192–200.
- 39. Mitchell RB, Archer SM, Ishman SL, et al. Clinical practice guideline: tonsillectomy in children (update). Otolaryngol Neck Surg. 2019; 160(1_suppl):S1–S42.
- 40. Collison PJ, Mettler B. Factors associated with post-tonsillectomy hemorrhage. Ear Nose Throat J. 2000;79(8):640–649.