A 65-year-old woman presented for evaluation of painful swelling of the face after routine dental extractions. Her medical history was significant for rheumatoid arthritis, for which she was taking prednisone 5 mg daily. Clinical examination revealed diffuse swelling of the right mandible/submandibular region, limited mouth opening, and paresthesia of the lower lip. Panoramic and computed tomography images revealed diffuse inflammatory changes of the right submandibular and submental spaces with osteomyelitis of the mandible (Figure 1). The patient was treated with preoperative antibiotic therapy followed by segmental resection of the mandible and reconstruction with a vascularized fibular graft.
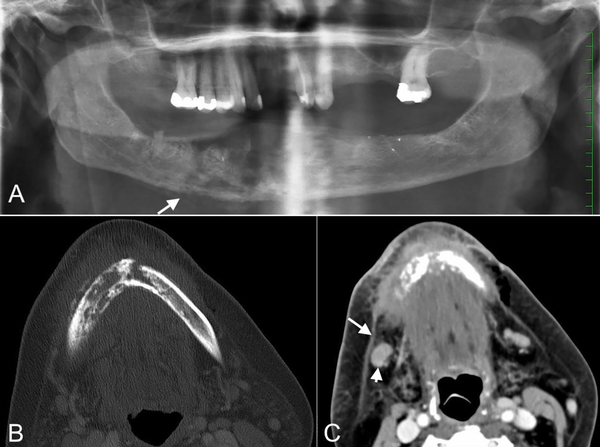
Figure 1
A, Panoramic radiograph shows a moth-eaten, permeative destruction of the right body of the mandible. Note the inflammatory periosteal reaction at the inferior border of the mandible (arrow). B, Axial CT image in bone algorithm shows a destructive lesion with a moth-eaten pattern. C, Axial contrast-enhanced CT image shows the changes of cellulitis in the submental region. There is thickening of the skin, “dirty” edematous fat in the subcutaneous soft tissues, thickening of the right platysma muscle (arrow), and level IB reactive lymphadenopathy (arrowhead). CT indicates computed tomography.
Osteomyelitis is an inflammatory process of the entire bone including the cancellous and cortical bone as well as the overlying periosteum. Osteomyelitis of the jaws usually results from an odontogenic infection; other factors such as extraction wounds, trauma, and radiotherapy have also been implicated as causative factors. Additionally, some diseases (eg, osteopetrosis, cemento-osseous dysplasia) may result in hypovascularized bone that is predisposed to necrosis and inflammation. Osteomyelitis occurs more commonly in the mandible than the maxilla, which may be related to the reduced blood supply to the mandible. Thick cortical plates and abundant medullary tissues in the mandible contribute to confinement of the infection within bone.
Clinical manifestations include pain, facial swelling, and limited mouth opening. Patients may have systemic symptoms such as fever, malaise, and lymphadenopathy. Involvement of the neurovascular bundle within the mandibular canal results in paresthesia of the lip.
The earliest radiographic change of osteomyelitis is a slight decrease in the density of the involved bone, making the trabeculae appear fuzzy. The trabeculae soon lose their continuity and bone resorption is more profound. In advanced cases, there are multiple foci of bone rarefaction and sclerosis with fragmentation or sequestration of bone. The bone changes are irregular and ill-defined and may be described as “moth-eaten.” The involved bone may produce laminated periosteal new bone formation. Pathologic fracture of the mandible may occur.
The differential diagnosis of osteomyelitis may include malignant lesions that can cause bone destruction and may stimulate a periosteal reaction (eg, osteosarcoma, squamous cell carcinoma, Langerhans’ cell histiocytosis). Sclerotic chronic form of osteomyelitis may be difficult to differentiate from fibrous dysplasia; however, a demonstrable cause for it usually exists.
Osteomyelitis of the jaws is caused by aerobic and anaerobic bacteria, including viridans streptococci, Peptostreptococcus, Fusobacterium, Prevotella, and Actinomyces. The treatment of osteomyelitis involves surgical debridement (eg, decortication, resection) with long-term antibiotic therapy.
Author’s Note Dr. Galal Omami is a Diplomate of the American Board of Oral and Maxillofacial Radiology.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
Galal Omami
https://orcid.org/0000-0003-1187-1816
References
- 1. Schuknecht B, Valavanis A. Osteomyelitis of the mandible. Neuroimaging Clin N Am. 2003;13(3):605–618.
- 2. Ida M, Tetsumura A, Kurabayashi T, Sasaki T. Periosteal new bone formation in the jaws. A computed tomographic study. Dentomaxillofac Radiol. 1997;26(3):169–176.
- 3. Petrikowski CG, Pharoah MJ, Lee L, Grace MG. Radiographic differentiation of osteogenic sarcoma, osteomyelitis, and fibrous dysplasia of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80(6):744–750.
- 4. Topazian RG. Osteomyelitis of the jaws. In: Topizan RG, Goldberg MH, Hupp JR, eds. Oral and Maxillofacial Infections. 4th ed. Saunders; 2002:214–242.
