Introduction
Tracheal and subglottic stenosis rates are likely on the rise following the COVID-19 pandemic. Anecdotally, we have seen an increase in rates of stenosis requiring open surgical resection at our institution over the past few years secondary to COVID-related morbidity in our region.
Complete tracheal transection is a rare, often life-threatening complication that can occur following tracheal injury. In most circumstances, complete tracheal transections occur following acute blunt - or penetrating, trauma. Typical symptoms include respiratory distress, subcutaneous emphysema, hoarseness or aphonia, hemoptysis, stridor, and loss of palpable landmarks. Iatrogenic transection from tracheotomy or tracheotomy tube exchange has not been described in the literature to our knowledge.
Here we present a “scary case” of a complete tracheal resection in a patient without a history of blunt or penetrating trauma. This injury was only recognized intraoperatively during tracheal dissection for anticipated tracheal reconstruction for presumed tracheal stenosis after COVID-19-related prolonged ventilation and tracheotomy. Herein we describe the presentation, operative findings, and management of this unusual and challenging case.
Case Report
A 32-year-old female with a past medical history only notable for asthma and psoriasis presented to an outside hospital in August 2021 due to COVID-19 and subsequently developed pneumonia requiring long-term mechanical ventilation. She received a PEG tube placement and bedside percutaneous tracheotomy. Upon weaning from ventilator support, she was found to be aphonic. Once stable, she was discharged to a long-term care facility.
She was seen by an outside interventional pulmonologist in November 2021, where she was noted to have evidence of tracheal stenosis and persistent aphonia. CT scan at that time revealed “mild costal thickening in the immediate subglottic region” and “soft tissue opacification of the airway approximately 2 cm below the glottis extending to roughly 7 mm proximal to the tip of the tracheostomy tube” (Figure 1). Bronchoscopy revealed complete tracheal stenosis with the presence of some central granulation in the subglottis.
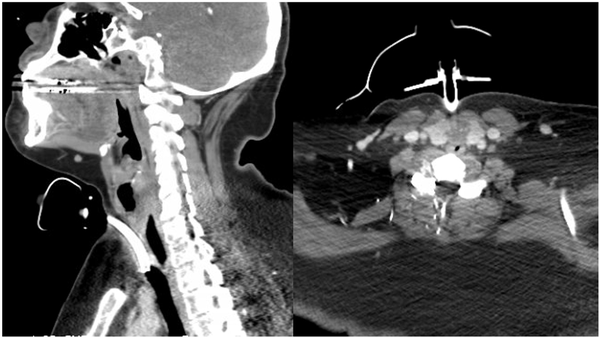
Figure 1
Computed tomography shows a 5.5 cm long cricotracheal stenosis extending from the cricoid to the tip of the tracheostomy (left) with complete opacification of the subglottic airway (right).
She was then referred to our tertiary care center for definitive open surgical resection by our multidisciplinary team. A review of imaging suggested a long segment of the involved trachea (>5 cm), so she has consented to tracheal resection with primary anastomosis and tracheal releases versus free flap reconstruction with a radial forearm and costal cartilage batten grafting.
During anterior neck exploration, after mobilizing the tracheostomy tract, she was noted to have a blind pouch at the inferior cricoid with no connection to the distal trachea (Figure 2). The tracheotomy tract was membranous tissue only. The first recognizable tracheal ring was below the sternum and located 5 cm from the inferior cricoid cartilage. The membranous tract was excised, and the trachea and larynx were mobilized with mediastinoscopy and suprahyoid release, respectively. After tracheal releasing techniques were completed, the trachea was found to be mobile enough to achieve a tension-free closure without free flap reconstruction. A tension-free anastomosis was then completed, and Grillo stitch was placed postoperatively.
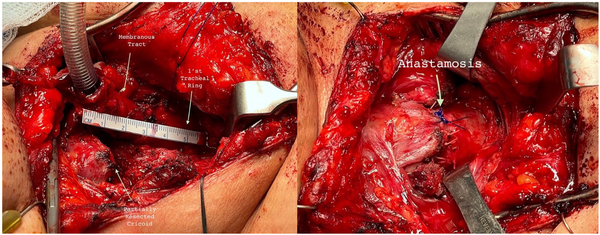
Figure 2
Intraoperative dissection at time of tracheal anastomosis. (Left) Distance from tracheostomy to first tracheal ring with a 5-cm, membranous tract connecting the tracheostomy to the distal trachea. (Right) Final anastomosis after mediastinoscopy and suprahyoid release with a complete tension free closure.
Postoperatively, she was cleared for a clear liquid diet on postoperative day (POD) 1. She was able to advance her diet as expected. The Grillo stitch was cut on POD 5. Clinical evaluation postoperatively was notable for a right vocal fold paralysis in a median position with good voice quality. She has continued to do well and has not required any intervention now, nearly 1 year out from surgery.
Discussion
This case is an example of complete tracheal transection in the setting of iatrogenic subglottic injury. To our knowledge, this is the first example of a complete tracheal transection after tracheotomy or tracheotomy tube exchange. As demonstrated in this case, our patient presented with chronic symptoms only notable for aphonia and tracheotomy dependence. She and her previous providers were unaware of the extent of her injury.
Tracheostomy is a common procedure, with over 50 000 to 80 000 tracheostomies completed in the United States each year. While common, it is important to acknowledge the procedural risks including bleeding (2%-5%), infection (0.5%), tracheal tube obstruction (0%-3.5%), and posterior membrane injury (6-50/10 000).
Injury to the posterior tracheal wall is a well-recognized complication of tracheotomy and has been noted to be higher in percutaneous tracheostomies over open tracheostomies. It is thought that most posterior tracheal wall injuries are a result of poor control of the guidewire and guiding catheter. While small injuries can heal without further intervention, larger injuries can present as airway bleeding, an air leak around the tube, or as seen in our case, provoke a complete transection.
Intraoperatively, our patient was noted to have a complete tracheal transection that we believe to be likely secondary to her tracheotomy and potentially further exacerbated by tracheostomy tube exchanges. Her intraoperative findings were notable for significant elasticity of the distal trachea and a lack of structural loss, suggesting that the airway dropped into the chest. The timing of transection, however, is unclear. It is feasible that it occurred at the time of trach placement or, alternatively, the lateral and posterior wall could have necrosed at the level of the ostomy, and the trachea could have subsequently dropped either in the postop period or with a trach change.
Typically, tracheal transection is an airway emergency that requires emergent surgical intervention to insert an endotracheal tube into the distal trachea. However, this case lacked the typical presentation of a tracheal transection with no acute respiratory distress or specific events to suggest the injury. This atypical presentation has been described in prior case reports with tracheal transection secondary to blunt trauma but has not yet been described in tracheal transection secondary to tracheotomy.,
Here we present a patient with a complete tracheal transection, without a history of blunt or penetrating trauma. While unusual, this case serves to suggest that transection can occur by tracheotomy or the postoperative care of a tracheotomy alone. It is important to recognize this as a potential entity in patients with presumed grade IV stenosis, as tube exchange could be particularly hazardous if the expected tracheal framework is not present.
Authors’ Note This research was presented at Cedar Sinai’s “Eerie ENT Cases” Conference.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
Andrew Yousef
https://orcid.org/0000-0002-3126-1655
References
- 1. Nitta K, Hamano Y, Kamijo H, et al. Complete cervical tracheal transection due to blunt trauma. Acute Med Surg. 2016;3(4):376–379. doi:
- 2. Seims AD, Shellenberger TD, Parrish GA, Lube MW. Cervical tracheal transection after scarf entanglement in a Go-Kart engine. J Emerg Med. 2013;45:e13-e16. doi:
- 3. Fleißner F, Timm ME, Lang CP, Lenarz T, Kühn C, Jaeger DB. Tracheal transection-A novel airway management. Thorac Cardiovasc Surg Rep. 2020;9(1):e24-e28. doi:
- 4. Chow JL, Coady MA, Varner J, Cannon W, Spain D, Brock-Utne JG. Management of acute complete tracheal transection caused by nonpenetrating trauma: report of a case and review of the literature. J Cardiothorac Vasc Anesthesia. 2004;18(4):475–478. doi:
- 5. Ishibashi H, Ohta S-i, Hirose M, Akimoto T. Blunt tracheal transection and long tear in posterior membranous trachea. Eur J Cardio Thorac Surg. 2006;30(6):945–947. doi:
- 6. Paik JH, Choi JS, Han SB, Jung HM, Kim JH. Complete cervical tracheal transection caused by blunt neck trauma: case report. Ulus Travma Acil Cerrahi Derg. 2014;20(6):459–462. doi:
- 7. Enomoto Y, Watanabe H, Nakao S, Matsuoka T. Complete thoracic tracheal transection caused by blunt trauma. J Trauma. 2011;71(5):1478. doi:
- 8. Hamid UI, McGuigan JA, Jones JM. Transection of the aerodigestive tract after blunt neck trauma. Ann Thorac Surg. 2011;92(5):1896–1898. doi:
- 9. Parage F, Vashisht A, Sisodia V, et al. Reconstruction of complete tracheal transection with cardiopulmonary bypass support following bull horn injury in neck during coronavirus disease 19 pandemic lockdown. Indian J Thorac Cardiovasc Surg. 2021;37(4):442–446. doi:
- 10. Dayal S, Dugom P, Kharazi A, et al. Tracheal transection from gunshot wound to the Neck. Ann Thorac Surg. 2022;114(1):e39-e41. doi:
- 11. Jean YK, Potnuru P, Diez C. Airway Management of near-complete tracheal transection by through-the-wound intubation: a case report. A A Pract. 2018;11(11):312–314. doi:
- 12. Fabre D, Kolb F, Fadel E, et al. Successful tracheal replacement in humans using autologous tissues: an 8-year experience. Ann Thorac Surg. 2013;96(4):1146–1155. doi:
- 13. Abril MK, Berkowitz DM, Chen Y, Waller LA, Martin GS, Kempker JA. The epidemiology of adult tracheostomy in the United States 2002-2017: a serial cross-sectional study. Crit Care Explor. 2021;3(9):e0523. doi:
- 14. Fernandez-Bussy S, Mahajan B, Folch E, Caviedes I, Guerrero J, Majid A. Tracheostomy tube placement: early and late complications. J Bronchology Interv Pulmonol. 2015;22(4):357-64. doi:
- 15. Moonsamy P, Sachdeva UM, Morse CR. Management of laryngotracheal trauma. Ann Cardiothorac Surg. 2018;7(2):210–216. doi:
- 16. Hosny A, Bhendwal S, Hosni A. Transection of cervical trachea following blunt trauma. J Laryngol Otol. 1995;109(3):250–251. doi:
