INTRODUCTION
Corticosteroids are a group of anti-inflammatory drugs that are used to treat various ocular and systemic diseases. Most of these are chronic conditions which require long term treatment. With the increase in environmental pollution there has been increased incidences of ocular allergy, URI, lung diseases, skin diseases which require steroid application in some form. Steroids have been considered as the magic drug of modern medicine but it is a double-edged sword. The over-the-counter availability of this cheap drug which causes immediate relief of symptoms has led to its misuse.
The use of steroids can lead to several ocular side effects. Steroid induced intraocular pressure elevation has been well documented
EPIDEMIOLOGY
Steroid induced IOP elevation can occur at all age groups. It has bimodal distribution. Very young (<10 years) and very old adults are at greater risk of steroid response. This accounts for one-fourth of all acquired glaucoma in children.[] Significant IOP elevations have also been reported in infants on inhalational and nasal steroids.
5-6% of normal patients show marked increase in IOP 4-6 weeks after steroid therapy. Thus 5% of the general population are steroid responders i.e their IOP increase after steroid administration. Becker and Armaly,, suggested three categories of steroid responders, based on IOP response to topical betamethasone and dexamethasone application: High responder, Moderate responder, Non-responder (table 1)
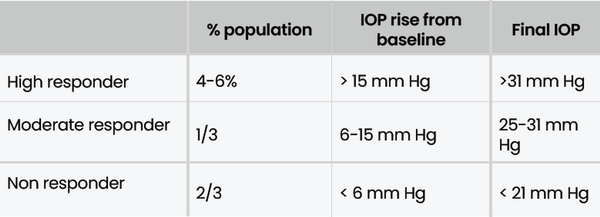
Table 1
Classification of Steroid Responders
ETIOPATHOGENESIS
Steroid induced glaucoma is a form of open angle glaucoma. The precise Mechanism of action is unknown clearly but primarily there is reduced facility of aqueous outflow.[] (figure 1) Glucocorticoids may exert their effect through increased expression of MYOC (TIGR) gene at locus GLC1A. Steroids cause stabilisation of the lysosomal membranes and accumulation of polymerised Glycosaminoglycans (GAGs) at the trabecular meshwork[,,]. These polymerised GAGs get hydrated causing biological oedema and increased ocular outflow resistance. Glucocorticoids increase the expression of extracellular matrix proteins fibronectin, GAGs, laminin, elastin which increases the blockage at the trabecular meshwork. They also inhibit the phagocytic activity of the endothelial cell lining the trabecular meshwork leading to accumulation of aqueous debris
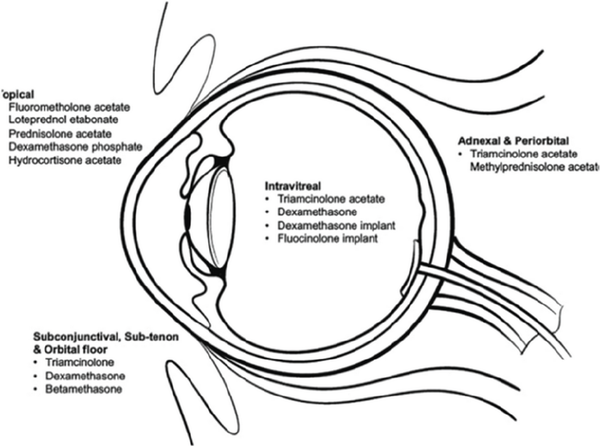
Figure 1
Etiopathogenesis of steroid induced IOP rise
RISK FACTORS
There are a certain group of patients who are at an increased risk of steroid induced IOP rise. Patients with POAG are at increased risk. 30% of Glaucoma suspects and 90% POAG might have a steroid induced ocular hypertensive response 4 weeks after topical dexamethasone 0.01% therapy. Normal individuals classified as high responders are most likely to develop POAG. First degree relatives of POAG patients (25-30%) are also considered to be at increased risk of developing steroid responder.
High Myopia or eyes with a history of Penetrating Keratoplasty, LASIK, PRK, DSEK are at increased risk of developing steroid induced IOP rise. Diagnosis of ocular hypertension is difficult in these cases because of thin CCT, ocular rigidity changes, corneal oedema, and accumulation of fluid beneath LASIK Flap.
Patients with Diabetes Mellitus, Connective Tissue Disorder (Rheumatoid Arthritis), Pigment Dispersion Syndrome, Traumatic Angle Recession, Endogenous Hypercortilsolism are at increased risk of steroid induced ocular hypertension.
ROUTES OF ADMINISTRATION
It has been documented that IOP can be increased by any exogenous routes of application of steroids.[] (figure 2)
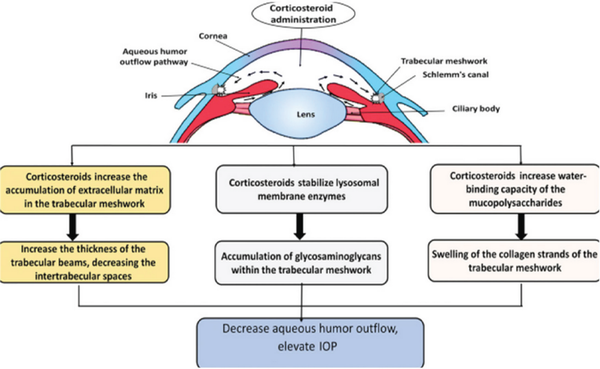
Figure 2
Steroid Induced Ocular Hypertension caused by various routes of administration of steroids
1. Topical therapy: IOP rise can occur more frequently with topical ocular therapy than systemic therapy. IOP rise can occur by drops or ointment either applied directly to eye or over the skin of the eyelids.
2. Periocular therapy: Periocular injection of repository steroids administered subconjunctival, sub tenons, and retrobulbar are the most dangerous form of steroids because of their prolonged duration of action. A patient’s response to topical steroid therapy does not predict their response to periocular therapy.[,]
3. Intravitreal therapy:
Intravitreal triamcinolone: IOP rise is a significant side effect after intravitreal triamcinolone therapy. According to a meta-analysis, percentage of IOP increase after intravitreal IVTA follows an inverted U-shaped pattern.[] (Table 2) In SCORE Study the cumulative rates of IOP elevation with IVTA (greater than 10 mm Hg above baseline within 36 months) were 2% for “standard of care”(no injection), 9% for patients treated with IVTA, 1 mg, and 45% for patients treated with IVTA, 4 mg. Patients should be monitored for 6 months for IOP management after IVTA injection.
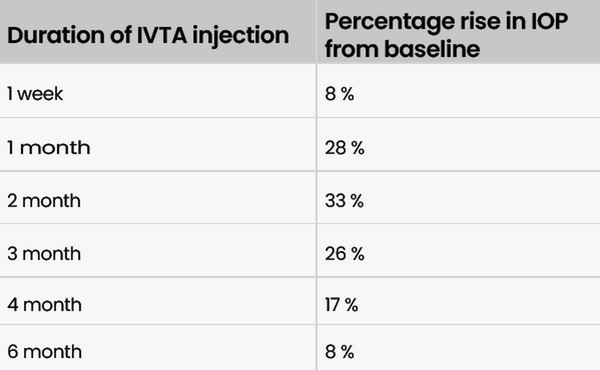
Table 2
IOP RISE AFTER IVTA INJECTION
Ozurdex (intravitreal dexamethasone implant): 12.6% of patients show an IOP increase >10 mm Hg from baseline after the first injection and 15.4% after the second dose of Ozurdex. The ocular hypertension is transient and less severe as compared to IVTA injection as Ozurdex is a more water-soluble steroid.[] Among patients treated with the 0.7-mg insert 41.5% required IOP-lowering medication and 0.3% required incisional surgery within 36 months
3. Systemic therapy: Systemic administration of steroids is the least likely route to cause IOP elevation. It may take longer duration to elicit an IOP rise after systemic therapy. If the pressure rises, the response does not correlate with the dosage or duration of treatment.
4. Inhalational steroids: Inhaled corticosteroid can lead to a rise of intraocular pressure. Even fluticasone propionate which has an excellent safety profile has shown to raise IOP in susceptible individuals.[] The risk of IOP rise is increased with higher dose and more puffs. Inhalational steroid induced ocular hypertensive response is common in patients with family history of glaucoma.
5. Face steroid creams can raise the IOP and irreversibly damage the visual field. If the applications are discontinued, the IOP typically falls after a lag phase, but glaucomatous damage may continue nonetheless. The duration of steroid use is important in the development of glaucoma.
The pressure-inducing effect of steroids is directly proportional to anti-inflammatory potency, dosage of the drug used duration of use. (Figure 3) Difluprednate is an effective topical corticosteroid, but it may cause dramatic elevation of IOP in some patients, particularly children.[] It can cause IOP increase even in those patients not previously considered to be steroid responders to other topical agents such as prednisolone acetate.
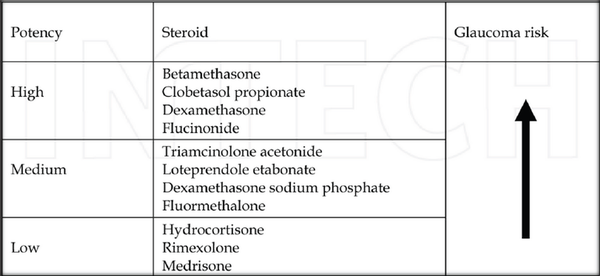
Figure 3
Comparison of pressure inducing effects of Steroids with Its potency
CLINICAL FEATURES
Steroid induced Glaucoma mimics Primary Open Angle Glaucoma. The IOP elevation is gradual with very few symptoms. History of systemic or ocular disease, which could require chronic corticosteroid use (e.g., uveitis, collagen vascular disease, asthma, dermatitis) should be elicited in all patients having ocular hypertension. The presenting symptoms depend on the age of the patient.
MANAGEMENT
Discontinuation of the steroid is the first line of management. In the majority of cases, IOP typically normalizes within days of stopping the steroid. In Chronic forms IOP decrease can take 1 to 4 weeks. The duration of steroid therapy also influence the reversibility of the IOP elevation. Corticosteroids like betamethasone, prednisolone, and dexamethasone can be substituted with nonadrenal steroids like rimexolone, loteprednol etabonate, fluorometholone, and medrysone. Steroids can be replaced with other steroid sparing medications like anti metabolites, NSAIDS, immunomodulators.
In rare cases where IOP does not normalise after stopping steroids, glaucoma therapy is required. Nearly all patients who develop steroid-induced iatrogenic glaucoma can be controlled with topical antiglaucoma therapy. By 6-18 months, most of the patients can be off medication. About 1-5% with intractable glaucoma may need surgery to normalize their IOP. The most commonly employed surgery in patients with virgin conjunctiva is Trabeculectomy. In cases of scarring shunt implantation or cyclodestructive procedures may be preferred. MIGS have also shown good results in these cases as the pathology is at the trabecular meshwork level. Excision in the case of sub-Tenon deposits and vitrectomy in the IVTA may be required in severe cases.
Prevention is better
Steroid induced glaucoma is a preventable disease. The unwarranted and irrational use of this magic drug should be avoided and self-medication should be strictly discouraged. The judicious use of steroids is advocated to make sure we find the best drug, the best concentration, the best frequency, the best route of delivery—which might be topical, peribulbar, intravitreal or systemic—and only have the patient use it as long as necessary under supervision.
The patients at risk should be identified and baseline IOP measurement be done to rule out preexisting glaucoma. IOP monitoring should initially occur at 2 weeks and then every 4-6 weeks for 2-3 months, and then every 6 months after an initial response has been ruled out. After cessation of steroid therapy, most eyes are off treatment at 18 months. Supervision for long periods is essential, as the IOP may rise even after initial control following cessation of steroids. Some common ocular allergies can easily be managed by Mast cell stabilisers, Anti allergic (olopatadine, bepostastine, alcaftadine). If required short course of low potency steroids under supervision should be given. Giving a steroid free window is necessary. Immunomodulators like cyclosporin A and tacrolimus can be used to substitute steroids. Chronic uveitis should be managed with NSAIDS (flurbiprofen, bromfenac, nepafenac) and antimetabolites like methotrexate giving steroid free window.
Thus, by following few practical and simple guidelines this iatrogenic disease can be averted.
FOOTNOTES AND DISCLOSURES
Financial disclosure
None
Conflict of Interest
None
Acknowledgements
Nil
REFERENCES
1.
Armaly MF. Statistical attributes of the steroid hypertensive response in the clinically normal eye.1: The demonstration of three levels of response. Invest Ophthalmol Vis Sci 1965; 14:187.2.
Armaly MF. The heritable nature of dexamethasone induced ocular hypertension. Arch Ophthalmol 1966; 75:32.3.
Becker B. Intraocular pressure response to topical corticosteroids. Invest Ophthalmol Vis Sci 1965; 4:198.4.
Birnbaum AD, Jiang Y, Tessler HH, Goldstein DA. Elevation of Intraocular Pressure in Patients With Uveitis Treated With Topical Difluprednate. Arch Ophthalmol. 2011;129(5):664-676. doi:10.1001/archophthalmol.2011.825.
Dang Y, Mu Y, Li L, Mu Y, Liu S, Zhang C, et al. Comparison of dexamethasone intravitreal implant and intravitreal triamcinolone acetonide for the treatment of pseudophakic cystoid macular edema in diabetic patients. Drug Des Devel Ther. 2014;8:1441-14496.
Francois J. Tissue culture of ocular fibroblast. Ann Ophthalmol 1975 Dec;7(12):1551-1554.7.
Francois J. The importance of the mucopolysaccharides in intraocular pressure regulation. Invest Ophthalmol Vis Sci 1975 Mar;14(3):173-176.8.
Francois J, Victoria-Troncoso V. Mucopolysaccharides and pathogenesis of cortisone glaucoma. Klin Monatsbl Augenheilkd 1974 Jul;165(1):5-109.
Fung AT, Tran T, Lim LL, Samarawickrama C, Arnold J, Gillies M, Catt C, et al. Local delivery of corticosteroids in clinical ophthalmology: A review. Clin Exp Ophthalmol. 2020 Apr;48(3):366-401. doi: 10.1111/ceo.13702. Epub 2020 Jan 22. PMID: 31860766; PMCID: PMC7187156.10.
Herschler J. Intractable intraocular hypertension induced by repository triamcinolone acetonide. Am J Ophthalmol 1972 Sep;74(3):501-504.11.
Herschler J. Increased intraocular pressure induced by repository corticosteroids. Am J Ophthalmol 1976 Jul;82(1):90-93.12.
Kaur S, Dhiman I, Kaushik S, Raj S, Pandav SS. Outcome of ocular steroid hypertensive response in children. J Glaucoma 2016 Apr;25(4):343-347.13.
Gaballa SA, Kompella UB, Elgarhy O, Alqahtani AM, Pierscionek B, Alany RG, et al. Corticosteroids in ophthalmology: drug delivery innovations, pharmacology, clinical applications, and future perspectives. Drug Deliv Transl Res. 2021 Jun;11(3):866-893. doi: 10.1007/s13346-020-00843-z. PMID: 32901367.14.
Nozik RA. Periocular injection of steroids. Trans Am Acad Ophthalmol Otolaryngol 1972 May-Jun;76(3):695-705.15.
Phulke S, Kaushik S, Kaur S, Pandav SS. Steroid-induced Glaucoma: An Avoidable Irreversible Blindness. J Curr Glaucoma Pract 2017; 11(2):67-72.16.
Rhee DJ, Peck RE, Belmont J, Martidis A, Liu M, Chang J, Fontanarosa J, et al. Intraocular pressure alterations following intravitreal triamcinolone acetonide. Br J Ophthalmol. 2006 Aug;90(8):999-1003. doi: 10.1136/bjo.2006.090340. Epub 2006 Apr 5. PMID: 16597664; PMCID: PMC1857192.17.
Sihota Ramanjit MD FRCS, Dada Tanuj MD, Rai Harminder K MD. Fluticasone propionate raises IOP in susceptible individuals. Indian Journal of Ophthalmology 52(2):p 170-1, Apr-Jun 2004.

