The United Nations (UN) has projected, by the year 2025, the total male population (above 60 years) is estimated to rise to 11% of the total world population, while the female population (above 60 years) to 13%. These figures are expected to take a bigger leap and reach 20% and 22%, respectively, by 2050. The UN classifies a nation as “aging” when the proportion of persons over 60 years crosses 7%, and India has made this transition faster than any other country in the world. In India, 2011 population census, there were nearly 104 million elderly persons (aged 60 years and above). Life expectancy rates rose from 32 years in 1947 to 65 years in 2011. The proportion of the elderly population, which was under 5%, rose to nearly 9%. As shown in a survey by the Census of India, NSSO, and UN in 2016, the trajectory of this transition is moving upwards, estimated an increase of elderly to 168 million in 2025 and a further 326 million by 2050. The transitions are fueled by falling mortality and fertility rates. The growth rate of the elderly is thrice that of the total population, implying the actionable moments are already passing, and there is a need to act fast.
The times of interdependence are on the wane as society embraces more and more urban values with reduced family sizes and increased individual autonomy. In total, 80% of the elderly reside in rural India, while a similar proportion of qualified mental health professionals reside in the urban areas, which places them at an access disadvantage. In this background of the crumbling informal support systems that arise due to demographic changes, there are enormously raised health risks to the elderly.
Mental Health and Geriatric Population
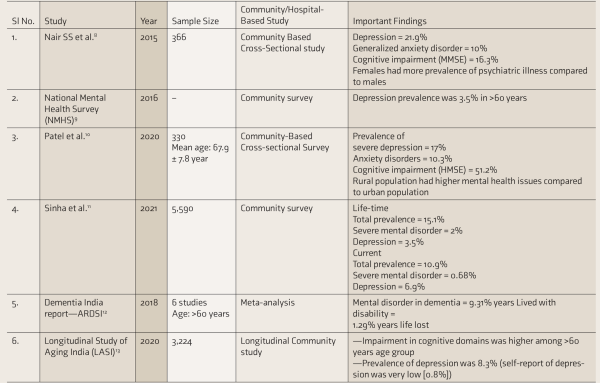
There is empirical evidence pointing to a decrease in the quality of life due to deterioration of mental health and generally poor physical well-being., Mental health challenges frequently co-occur with physical health conditions among the elderly. The prevalence of psychiatric illnesses is higher (Table 1). Most studies are hospital-based or conducted in smaller cohorts in the community. GMH problems are often attributed to “normal aging” inaccurately by HCPs and families. There is also stigma related to mental illnesses, which often leads to reluctance in seeking care, further deepening the gap.
The geriatric population is susceptible to many medical conditions, and it has been seen that elderly with psychiatric illnesses often have medical comorbidities, and vice versa., Therefore, it is pertinent that Care Models for the elderly need to incorporate services and make provisions keeping in mind the various levels of infirmity, disability, and assistance required by the elderly.
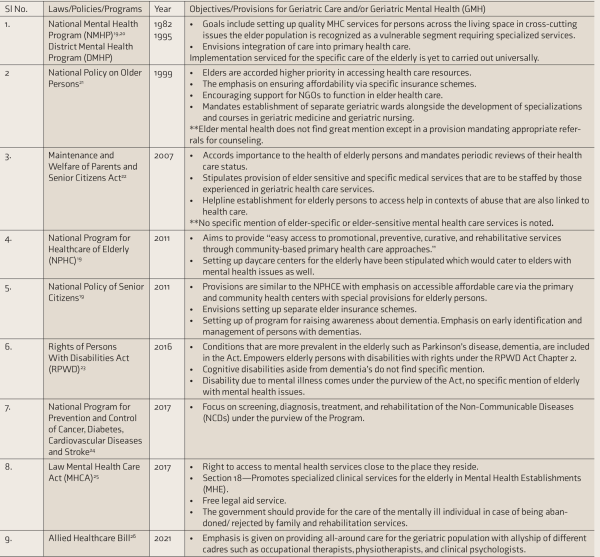
Legal Mandates, Policies, and Programs for the Care of Elderly
The well-being of senior citizens is mandated in the Constitution of India under Article 41, “The state shall, within limits of its economic capacity and development, make effective provision for securing the right to public assistance in cases of old age.” In Table 2, we describe the various laws, policies, and programs in India that address the issues of the geriatric population and the provisions for general and/or mental health care of geriatric population.
Current Infrastructural Resources for GMH Care
Care for the elderly with mental health challenges are provided in four types of setting: General hospital psychiatry settings, which include government and private hospitals/medical colleges, private and government psychiatric hospitals, NGOs, (like HelpAge India, ARDSI among others), and informal sources—family as caregivers., The largest care resource is the beleaguered family, who are the informal caregivers. There are only two institutions at present that offer exclusive superspecialization training in GMH in India, with a mere four geriatric psychiatrists as DM trained yearly.
Services range from acute care management to long-term care.
Acute care is provided mostly in hospital settings.
Memory clinics, specialized clinics that offer clinical assessment, support, information, and advice to persons with memory problems concentrated in the urban settings and Centers of excellence. ARSDI has even put forth guidelines for the establishment of such clinics.,
Day care centers; residential care facilities, which may be long term care or short-respite care.
Domiciliary care services at the residence, such as caregiver training, formal nursing care provided by geriatric home nurses, or other trained personal.
Support groups for families.
Dementia helpline (phone lines handled by trained personnel to address the queries on dementia).
It is important to note here that primary care for GMH care is practically nonexistent in our country.
Current Human Resources for GMH Care
HCPs in India range from super specialists to community health workers to volunteers from the community. As of April 2021, about 1,266,942 MBBS doctors have registered with various states. In 2018 more than 75% of the registered doctors are practicing as GP., The NMHS 2015–16 reported there are a mere 0.3 psychiatrists, 0.07 psychologists, and 0.07 social workers per 100,000 people in India. As of 2019, it was about 9,000 and counting, with 700 psychiatrists joining the league every year. Going by these figures, India has 0.75 psychiatrists per 100,000 populations, while the desirable number is anything above 3 psychiatrists per 100,000. MD-geriatric medicine offered in about ten institutions across the country includes cognitive assessment and identification of CMDs in inclusive; however, they are concentrated in a few private medical colleges and INIs. Further, DM—GMH/DM in geriatric psychiatry is very less (four per year). About 14 lakh nurse/midwives, about 5 lakh AYUSH medical professionals, and 8 lakh ASHA workers. Health care workforces are not trained adequately for GMH care.
Future Directions
The elderly population in mental health care has been considered a special population whose care is often considered possible only at higher centers such as medical colleges or MHE or institutes of reputes.
Quality GMH care is a multidisciplinary intensive team-based effort. Service provision needs to have adequate (a) depth: the extent to which conditions can be cared for, (b) breadth: the number of conditions that likely be serviced, and (c) length: the population to whom this would be accessible. At each stage of the current health care system, it is imperative to incorporate policy thoughts and approach strategies to the challenges foreseen while keeping in mind the available resources. Accordingly, a stepped care approach for GMH care is recommended. We propose a bottom-up approach (Figure 1) to GMH care, wherein community care, that is, primary care, forms the foundation and basis for addressing GMH needs while INIs are the last stop for GMH care.
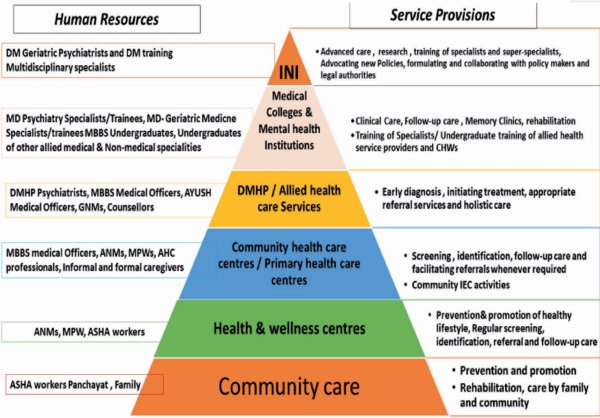
A Bottom-up Approach to Geriatric Mental Care—Human Resources and Service Provisions
Scaling Up Infrastructure
Training and scaling up human resources must go hand-in-hand with developing the infrastructure, and policies regarding the GMH should be developed with a multidisciplinary lens.
Enhancing infrastructural capacities should occur at all levels of Health care; some of the solutions/suggestions include:
Geriatric Care in Primary and Community Health Centers (PHCs, CHCs) and Secondary Hospitals: As Shown in the Pyramid (Figure 1)
GMH care should begin at the community level itself, and further care should be provided at the level of the PHCs and CHCs,
Should provide for promotion and prevention and regular screening for early diagnosis and follow-up care.
Community-based intervention programs that proactively link elders with challenges to the nearest PHC/CHC. Proactive case management approach to be created by CHWs such as ASHA workers.
Community care for dementia and provision of formal care closer to their place of residence should be established. AHC Professionals and/or Nurses could staff Day care programs and centers.
Low-cost dementia care homes, specifically for those with moderate or severe dementia, would be vital for elders living alone or those whose families cannot take care of them anymore.
Collaborative activities across various health programs such as NPCDCS and NMHP and other health programs should also be made to strengthen the existing health systems at community care.
District Hospital—District Mental Health Program (DMHP)
The focus should be on both prevention/promotional and providing acute care and follow-up care for GMH care.
Every DMHP should have an exclusive OPD to address GMH care in the elderly; this would be an important upgrade in the existing infrastructure as more than 800 districts across the country have implemented DMHP.
Services should enable integrated clinical settings to bring together physicians and psychiatrists to provide holistic geriatric health care.
NPCDCS also envisaged integrating all frontline workers and AYUSH in implementing the program’s objectives, thereby catering to both preventive, early diagnosis, and treatment of NCDs,, thus including AYUSH professionals will add to holistic GMH care.
Exclusive beds should be allotted for the care of elderly with mental illness, which can be part of the psychiatry beds or medical beds allotted for elderly patients.
Allied Health Care (AHC)
Due to its intersectional nature, improvement in GMH care would require inputs from various disciplines.
The National Commission for Allied and Healthcare Professions Bill (2021) highlights the provisions of inputs from different health care professions, such as physiotherapy, occupational therapy professionals, and community care (such as community health promoters, ecologist), behavioral health sciences (such as psychologists, social workers) and other professionals (such as a podiatrist, palliative care professionals).
Training the AHC professionals in GMH will enhance GMH care.
Medical Colleges and MHEs
Medical colleges and MHEs should have provision for GMH care, rather than serving as a conduit to higher centers.
Recently, a major change was made in the curriculum for MBBS graduates by NMC. The new competency-based MBBS curriculum enforced from 2019 has increased the duration of exposure for psychiatric training of medical students; however, not skill in psychiatry is required for licensing and successful completion of MBBS training.
Enable multidisciplinary care of elderly with mental health issues or dementia. An OPD dedicated to geriatric care services to provide integrated care is the need of the hour. This would enable both care and adequate training and clinical exposure for UGs and PGs. Collaborative care between geriatric medicine specialists and psychiatrists will enable this model to function without additional burden on the existing resources.
Setting up a memory clinic at every medical college/MHE is essential to address the Mental health needs of rising numbers of elderly with dementia.
Minimum ten inpatient beds should be allotted for tertiary geriatric psychiatry care serving dual care and training purposes.
Institutes of National Importance (INIs)
Each state should have an INI; INIs should have specialized centers for diagnosis and plan care evaluations of neuropsychiatric conditions in the elderly.
INIs should be equipped with facilities to enable research and innovations.
INIs need to take up the role of Zonal level specialty centers to enable capacity building and collaborative activities.
INIs need to function as advisories for policymakers to improve existing provisions and establish new ones.
Scaling Up Human Resources
Shortfalls in human resources are already impacting the access and service gaps for various health care services and many other factors. Current numbers are woefully inadequate; DM cadre is the central cog for health care machinery dedicated to geriatric mental health. It is prudent to incorporate a greater degree of training and exposure to mental health issues for all HCPs. There is a need to augment the apex numbers for diagnostic evaluation care plan formulation. Training super specialists without an adequate workforce at primary care will be futile.
Training of Caregivers and Family Members
Caregivers play an important role in managing the disability of the elderly; it is of utmost importance to increase the number of community-based old age homes and nursing homes for the elderly without caregivers. Though MHCA 2017 comments on the availability of community-based rehabilitation services for special populations, no advances have been made in that direction. The CHWs should also provide training to caregivers to assist the elderly, address their burden and deal with the loss.
Community Leaders
Community leaders and local NGOs should be included in the workforce to implement the national health programs. They should be trained in identifying the needs of the elderly and provide them basic counseling for referral, thereby bridging the treatment gap and lack of awareness of GMH needs.
Capacity Building of Existing Personnel at All Levels—CHWs, ANMs, etc.
At the subcenter/health and wellness center, special emphasis is made on health promotion and early identification. Along with NCD, it also focuses on mental health, neurological, substance use disorders, and memory impairment in the elderly.
Care should include high-risk populations in the screening, that is, elderly with a disability, elderly with existing mental illness, LGBTQ elderly, and elderly with abuse. Screening tools should be formulated to identify common mental disorders among the elderly and basic counseling skills to address this issue.
AHC Professionals
The elderly population is at increased risk of multiple morbidities leading to disability. In total, 13% of the elderly suffer from at least one type of disability that hampers at least one activity of daily living. This disability ranges in the form of vision, hearing, walking, and memory. Multimodal management is required to address this disability.
To date, the expertise would come with experience. Still, AHC courses should be planned for geriatric care for nurses, psychologists, social workers, and physical therapists to handle these special needs of the elderly.
Traditional and Alternative Medicine Practitioners
Ministry of AYUSH is formed to provide focused attention to the development of Education and Research in Ayurveda, Yoga, Naturopathy, Unani, Siddha, and Homoeopathy. These alternative medicine practices focus on healthy life and longevity. AYUSH and other integrated services should be encouraged at all the level of health care. Special fellowship programs should be planned for training them in geriatric health problems and manage multiple disabilities.
Creation of a Separate Cadre of Psychiatric Nurses
High-income settings have a specialized “geropsychiatric nursing” cadre with independent technical standards.
Incorporating short-term training programs for all nursing professionals and a specific posting for geriatric care in general and geriatric mental health during the undergraduate training will be essential to make them sensitive and aware of the GMH needs.
Undergraduate MBBS Students Training
With the horizontal inclusion with other specialties like medicine and pediatrics during the psychiatry training, we may see a change in the integrated learning in MBBS. Training in psychiatry and orientation to geriatric psychiatry topics in MBBS is important in itself, as many would take specialization when they would cater to the care of the elderly. Early sensitization toward the needs of the geriatric population, both physical health and GMH, will help in reducing the treatment gap and provide the services at the primary level.
Training of GPs
Even though GPs shoulder much of the medical care for the elderly, their training curriculum is still focused much on general health and a bit of palliative treatment of the geriatric population only. Therefore, training for GPs in GMH should focus on prevention, identification of early signs of psychiatric illnesses and cognitive impairment, and risk factors.
Continuum of Medical Education, workshops, diploma courses, and fellowship programs addressing their knowledge, attitude, and practices toward GMH issues is required.
For government-employed GPs, funds should be allocated for training and collaborative activities.
Training of Gerophysicians
Gerophysicians are a valuable addition to geriatric care; more than ten institutes provide MD. Geriatric medicine offers comprehensive services like comprehensive geriatric assessment (disability, incontinence, frailty, fall & injury risk, depression, and memory), supportive care, palliative care, rehabilitation, and healthy aging counseling. This specialty, a recent inclusion in the PG courses, maybe an ideal health resource for GMH.
Training of Psychiatrists
Psychiatrists need to cater to children, adolescents, adults, and elderly populations, and elderly need to compete with other populations to seek help. Additionally, most trained psychiatrists receive inadequate training in geriatric psychiatry during their PG training and ultimately do not feel competent enough to manage elderly patients.
A dedicated posting for geriatric psychiatry in all postgraduate psychiatry residency programs need to be introduced. Special evaluation and research should be planned to focus on GMH.
They should also be involved in the training of paraprofessionals.
Training Geropsychiatrists
Scaling up the super-specialty health professionals is the utmost requirement looking at the current scenario that shall provide advanced care and research for innovations and advancements in GMH, including Dementias’.
Training of Policymakers/Advocates/Judges
Training of HCPs and research alone is not enough to bring change. Policymakers themselves must be involved in understanding the needs elderly, especially the mental health needs.
Research findings must communicate to policymakers and others to make enhancements and changes in the existing systems.
Fine-Tuning Policy Mandates, Legal Provisions, and Programs
For any policy change to occur, it is essential to recognize the burden both to individuals, the community, and the economic burden at large due to GMH issues.
Social Security Measures
Schemes both disability and welfare schemes should be promoted to prevent neglect and abuse of the elderly, empowering them for independent living.
Pension schemes for senior citizens should be disbursed to all vulnerable groups among elderly.
Health care provider awareness of such schemes and active participation by all stakeholders (elderly to the policymakers) should be encouraged in planning processes.
Vocation options and community engagement should be encouraged.
Setting up legal aid clinics in all district headquarters and educating all stakeholders about the legal provisions available for elderly.
Like the “VAYOMITHRAM” a government social-security scheme for the elderly in Kerala, several schemes already exist. It provides social security for the elderly in free medication, financial assistance, and rehabilitation. Similar schemes providing holistic care can be adopted for the elderly with the inclusion of those with mental illness.
Policy and Programs
Building the NPHCE and including mental health as a priority. Further harmonize it with national mental health policy to include GMH as a priority issue in the NMHP, District Mental Health Program, and other NCD programs.
Adequate budgetary allocations for GMH within health care and mental health care budgets. Allocations need to be evenly and equitably distributed for community-based and facility-based interventions.
Creation of a special task force to review training and program implementation periodically every 3–5 years. The task force should be involved in training; help in updating the information, and including their experience and community needs in the training modules.
Envisioning the Horizon
The Health and Aging Policy Fellowship is a training strategy adopted by high-income settings to improve geriatric care policy and its implementation.
Supervised by experienced geriatric clinicians and training fellows from various disciplines to collaborate and produce more holistic policies for the geriatric population. Alongside training aspects, they are to assist legislators in tweaking policies. They perform service audits and report scope for improvement. Over a decade, more than 100 fellows have been trained on improving the implementation of geriatric care programs. This cadre can be a source of advisory support over long periods., A similar cadre would greatly benefit GMH policy planning and implementation.
A single national policy for elderly should be constituted to include all aspects of elderly, ranging from physical, mental health, protection and promoting well-being under one program/policy rather than diversifying into various programs/policies and laws.
Conclusions
The authors have made a case for the urgent need to act in a multipronged manner toward empowering the national health care systems to handle the demographic transitions and the looming GMH crisis. Concurrent efforts in multiple directions are required to address this challenge. They are scaling up specialized and nonspecialized human resources, scaling up infrastructural resources at all levels from health and wellness centers to zonal/apex centers for research and complex case management, and the rollout of relevant social measures to empower and enable the elderly. The coronavirus disease-19 pandemic has shown us the need to focus on the elderly. Community care is best for protecting the elderly; within this community care framework, we need to plan for future GMH care needs.
Urgent, affirmative, and substantial measures ought to be taken sooner rather than later. Therefore, we must take necessary steps for better preparedness to address the needs of our aging population.
Declaration of Conflicting Interests The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. United Nations. World Population Ageing (Highlights), 2019. New York: Department of Economic and Social Affairs, Population Division, 2019.
- 2.
- 3. National Sample Survey Organisation. The aged in India: a socio-economic profile: NSS Fifty-second Round, July 1995-June 1996. National Sample Survey Organisation, Department of Statistics, Ministry of Planning & Programme Implementation, Government of India, 1998.
- 4. Lodha P, De Sousa A. Geriatric mental health: the challenges for India. J Geriatr Ment Heal, 2018; 5(1): 16–29.
- 5. Katiyar RV, Ahmad S, Beg MW, . Geriatric mental health challenges in India—a review. J Evol Med Dent Sci , 2020; 9(23): 1787–1794.
- 6. Steverink N, Westerhof GJ, Bode C, . The personal experience of aging, individual resources, and subjective well-being. J Gerontol B Psychol Sci Soc Sci , 2001; 56(6): 364–373.
- 7. Furstenberg A-L. Trajectories of aging: imagined pathways in later life. Int J Aging Hum Dev , 2002; 55(1): 1–24.
- 8. Nair SS, Raghunath P, Nair SS. Prevalence of psychiatric disorders among the rural geriatric population: a pilot study in Karnataka, India. Cent Asian J Glob Heal , 2015; 4(1): 138.
- 9.
- 10. Patel M, Bhardwaj P, Nebhinani N, . Prevalence of psychiatric disorders among older adults in Jodhpur and stakeholders perspective on responsive health system. J Fam Med Prim Care, 2020; 9(2): 714–720.
- 11. Sinha P, Hussain T, Boora NK, . Prevalence of common mental disorders in older adults: results from the National Mental Health Survey of India. Asian J Psychiatr 2021; 55: 102463.
- 12.
- 13. Yogiraj Khobragade P, Banerjee J, Angrisani M, . Design and methodology of the longitudinal aging study in India-diagnostic assessment of dementia (LASI-DAD). J Am Geriatr Soc, 2020; (suppl 3): S15–S20.
- 14. Bhushan Tyagi B, Kalyan Mohanti B, Kumar Bhardwaj N, . Profile of common morbidities among geriatric population attending at a new tertiary care institute. Int J Med Heal Res [Internet], 2017; 3(4): 31–42.
- 15. Grover S, Avasthi A, Sahoo S, . Prevalence of physical comorbidity and prescription patterns in elderly patients with depression: a multicentric study under the aegis of IAGMH. J Geriatr Ment Heal, 2018; 5(2): 107–114.
- 16. de Lima JD, Teixeira IA, Silva F de O, . The comorbidity conditions and polypharmacy in elderly patients with mental illness in a middle-income country: a cross-sectional study. IBRO Rep December, 2020; 9 96–101.
- 17. Kumar K, Kar S, Reddy P. Psychiatric comorbidity in geriatric inpatients. J Dr NTR Univ Heal Sci, 2012; 1(2): 81–85.
- 18. Grover S, Dalla E, Mehra A, . Physical comorbidity and its impact on symptom profile of depression among elderly patients attending psychiatry services of a tertiary care hospital. Indian J Psychol Med , 2017; 39(4): 450–456.
- 19. Verma R, Khanna P. National program of healthcare for the elderly in India: a hope for healthy ageing. Int J Prev Med, 2013; 4(10): 1103–1107.
- 20.
- 21. Government of India. The National Policy on Older Persons. New Delhi: Government of India, Ministry of Social Justice and Empowerment, 1999.
- 22. Government of India. The Maintenance and Welfare of Parents and Senior Citizens Act. New Delhi: Government of India, 2007.
- 23.
- 24. Kumar Raina S. From NHM to NPCDCS: epidemiological transition and need for a national program for diabetes in India. J Metab Syndr, 2016; 5(2): 1–3.
- 25.
- 26. Singh O. The National Commission for Allied and Healthcare Professions Act, 2020 and its implication for mental health. Indian J Psychiatr, 2021; 63(2): 119–120.
- 27. Murali T, Tibrewal PK. Psychiatric rehabilitation in India. Ment Heal Care Hum Rights, 2008; 197–204.
- 28. Prakash O, Kukreti P. State of geriatric mental health in India. Curr Transl Geriatr Exp Gerontol Rep , 2013; 2(1), 1–6.
- 29. ARDSI. ARDSI guidelines for establishing memory clinics. Kerala: ARDSI, Government of Kerala, 2015.
- 30. Varghese Babu, Abraham Mathew, Sudhir Kumar CT. Memory clinics—a model for dementia care. IP Indian J Neurosci , 2020; 4(2): 48–51.
- 31.
- 32. Sagar R, Pattanayak R. Suicidality and mood disorders: gatekeepers’ training and mental health first aid. J Ment Heal Hum Behav, 2016; 21(2): 85–87.
- 33. Laxminarayan R. The economics of general practitioners: time for India to lead tech breakthrough in primary healthcare. Financial Express, 30 March, 2020.
- 34. Garg K, Kumar CN, Chandra PS. Number of psychiatrists in India: baby steps forward, but a long way to go. Indian J Psychiatr, 2019; 61(1): 104–105.
- 35.
- 36. Karan A, Negandhi H, Hussain S, . Size, composition and distribution of health workforce in India: why, and where to invest? Hum Resour Heal , 2021; 19(1): 1–14.
- 37. Pinkas J, Gujski M, Humeniuk E, . State of health and quality of life of women at advanced age. Med Sci Monit , 2016; 22 3095–3105.
- 38.
- 39. Stein DJ, Benjet C, Gureje O, . Integrating mental health with other non-communicable diseases. BMJ [Internet] , 2019; 364: l295. http://www.bmj.com/content/364/bmj.l295.abstract
- 40. Kishor M, Gupta R, Ashok M, . Competency-based medical curriculum: psychiatry, training of faculty, and Indian psychiatric society. Indian J Psychiatr, 2020; 62(2): 207–208.
- 41. Singh H. Perspectives in innovation in the AYUSH sector. J Ayurveda Integr Med, 2011; 2(2): 52–54.
- 42. Robinson KM. Policy issues in mental health among the elderly. Nurs Clin N Am, 2010; 45(4): 627–634.
- 43. Grover S. Future of psychiatry in India: geriatric psychiatry, a specialty to watch out. J Geriatr Ment Heal, 2014; 1(1): 1–5.
- 44. Otten JJ, Dodson EA, Fleischhacker S, . Getting research to the policy table: a qualitative study with public health researchers on engaging with policy makers. Prev Chronic Dis , 2015; 12(4): 1–8.
- 45. Cacchione PZ, Pike KM, Spaeth–Rublee B, . Health and aging policy fellows: Dementia and mental health policy to improve lives of older adults. J Am Geriatr Soc., 2018 ; 66: S53–57.
- 46. Pincus HA, Pike KM. Health and aging policy fellows: training future leaders to address geriatric mental health. Am J Geriatr Psychiatr, 2018; 27 178–180.