1 INTRODUCTION
Treatment, cleansing, moisturizing, and photoprotection constitute the four major components of skin care routine for dermatological conditions. While therapeutic guidelines for the management of atopic dermatitis, acne, and rosacea exist, there is a lack of practical recommendations on the importance of cleansing, moisturizing, and photoprotection (“CMP”). Despite an increasing demand for these skincare products, there are several unmet needs and challenges in the implementation of CMP in clinical practice.
About 40% of consumers are purchasing skincare products upon the recommendations of acquaintance rather than base on dermatologists' guidance. Limited patient knowledge of skin condition, lack of educational materials, and inadequate time for patient education during dermatological consultations, are the main obstacles to establishing a CMP routine in holistic skin care routine., Additionally, the wide range of over‐the‐counter (OTC) skincare products with different compositions is overwhelming for patients and hinders appropriate product selection. This is reflected in the high incidence of side effects (23.8%) associated with the inappropriate use of skincare and cosmetic products.
Most patients consider dermatologists as the highly trusted source of information on skin care product recommendations and expect dermatologist guidance on proper use of products. Patients are four times more likely to follow dermatologist's direction when product information is provided. Patient education is a crucial factor in promoting patient compliance and communication with dermatologist is an important element driving patient satisfaction, implying the need for dermatologist guided skin care routine.
Although treatment, cleansing, moisturizing, and photoprotection are the four major components of holistic skin care plan for the management of dermatological conditions, therapeutic treatment is the key component. Nevertheless, inclusion of recommendations on therapeutic management of acne, rosacea, and atopic dermatitis is beyond the scope of this publication, which have been published elsewhere. It is beyond doubt that holistic skin care should focus on therapeutic treatment first while considering individual skin differences and understanding product details to include cleansing, moisturization and photoprotection in accordance with different stages of the disease course. However, there is a lack of practical guidance on the role of cleansing, moisturizing, and photoprotection in holistic skin care. To fulfill this unmet need, this paper aims to focus on the adjunctive role of CMP in alleviating signs and symptoms of the skin conditions and improving quality of life.
2 METHODOLOGY
This study aimed to review current clinical evidence, identify gaps, and provide practical guidance on the implementation of holistic skin care routine in the management of sensitive skin conditions as observed in acne, atopic dermatitis, rosacea, and idiopathic sensitive skin syndrome, since these are among the most encountered skin conditions in clinical practice in the Asia Pacific region.
Sensitive skin syndrome is a condition characterized by stinging, burning, pain, pruritus, and tingling sensations in response to stimuli that normally should not elicit such sensations. These unpleasant sensations cannot be explained by lesions attributable to any skin disease. Sensitive skin syndrome may be seen in conditions such as acne, atopic dermatitis, or rosacea or it may be idiopathic without any underlying skin conditions. Due to its complexity, the diagnosis and treatment of sensitive skin are beyond the extent of this paper; instead, we focus only on CMP components of holistic skin care for sensitive skin syndrome.
An expert panel comprising of 10 dermatologists from Australia, China, Hong Kong, Taiwan, India, Indonesia, Philippines, Singapore, South Korea, and Thailand was selected based on their dermatological experience and expertise. The panel conducted a PubMed literature search and extracted articles in English published between January 2010 and October 2020. Search terms used were “atopic dermatitis,” “acne vulgaris,” “rosacea,” “sensitive skin”, “skin care,” “patient education,” “practice guidelines,” “skin cleansing,” “emollients,” “moisturizers,” “photoprotection,” “sunscreens,” “sun protection factor,” and “detergents.” The panel drafted consensus statements on holistic skin care in acne, rosacea, atopic dermatitis, and sensitive skin syndrome. Publications were prioritized with guidelines from international society and expert opinions considered to provide the highest level of evidence, followed by randomized controlled trials, reviews, and clinical case studies.
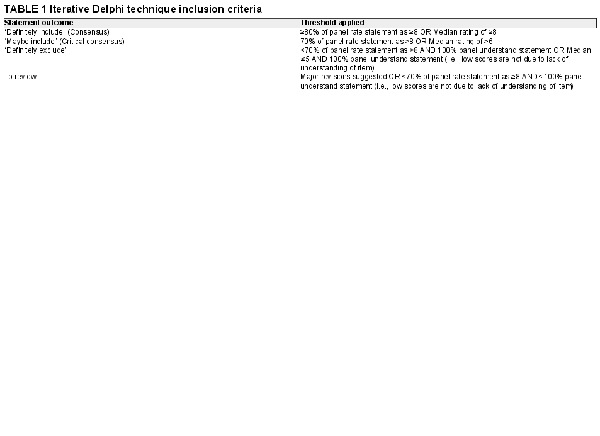
An iterative Delphi approach was employed to develop consensus as per the Delphi inclusion criteria. (Figure 1 and Table 1).
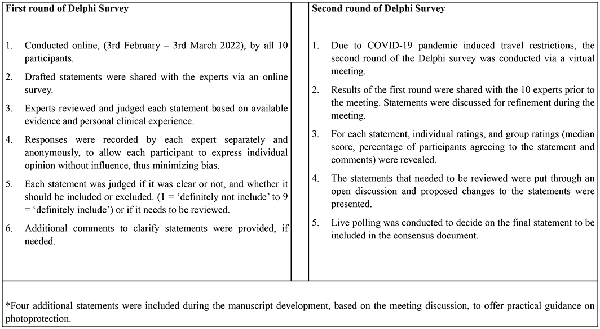
FIGURE 1
Delphi Survey Process of consensus generation and refinement
3 RESULTS
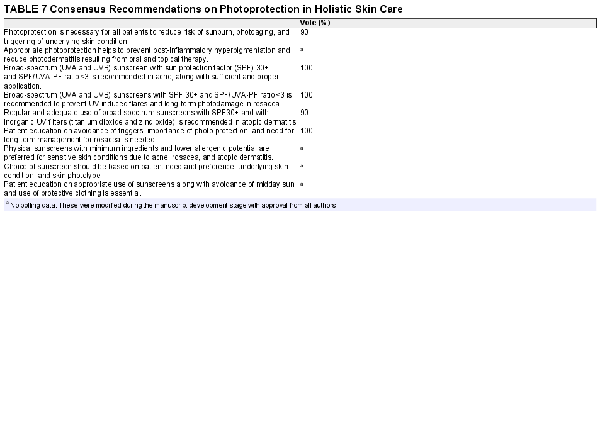
Based on the literature search results, the panel drafted 46 consensus statements which were included in the iterative Delphi approach survey. Of the 46 draft statements, 18 statements obtained a threshold of “definitely include” (median score of ≥8, OR ≥ 80% of panel rate as ≥8), while 24 statements needed discussion and refinement as they fell into threshold of “to review” despite obtaining a threshold of “definitely include” (for e.g., median score ≥7, but <70% of panel rate as ≥8 and <100% of panel understand statement). Four statements were in the category of “definitely exclude” (i.e., median score ≤5 and 100% of panel understand statement, low scores are not due to lack of understanding of item) Table 1. The statements selected for refinement were discussed and finalized through live voting. Five statements with similar meaning or content were deleted, and 4 additional statements on photoprotection were added to generate a final of 41 statements, which were collated to develop consensus recommendations on holistic skin care in sensitive skin syndrome associated with acne, atopic dermatitis, rosacea, and idiopathic sensitive skin syndrome. The process of refinement of statements is shown in Figure 2 The statements are presented in Tables 2, 3, 5 and 7.
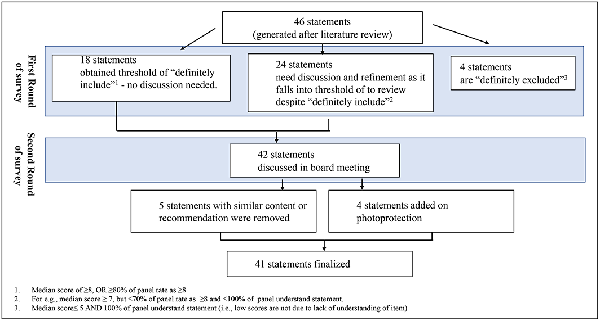
FIGURE 2
Generation and refinement process of recommendation statements
4 DISCUSSION
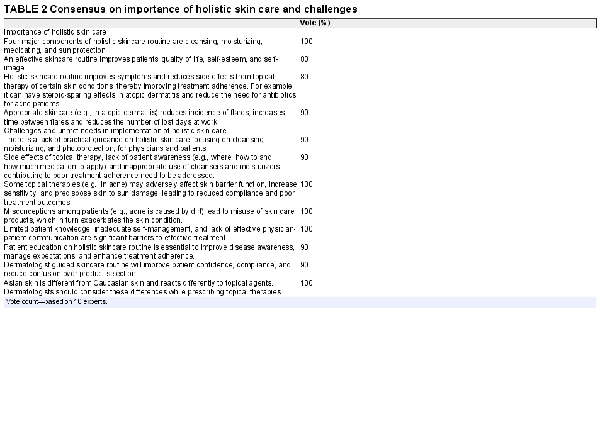
4.1 Challenges in implementation of holistic skin care
The expert panel emphasizes the importance of CMP components of holistic skin care and highlights the unmet needs, particularly, the lack of practical guidance, for both patients and physicians on the implementation of CMP routine in clinical practice, as outlined in Table 2. Limited patient knowledge about the skin conditions, time constraints of busy dermatological practices limiting patient education opportunities, and overwhelming choice of OTC products increase the risk of inappropriate use of skin care products, and hamper treatment outcomes., For example, side effects such as dryness, irritation, and photosensitivity are the main reasons for poor patient compliance with acne therapy. Paucity of patient guidance on the appropriate use of CMP routine to mitigate these side effects is a significant hurdle in improving patient compliance. Based on the clinical experience, the panel highlights the lack of patient understanding on how to choose and use CMP in conjunction with pharmacological therapy, how to avoid triggers, and how to use sun protection as major unmet needs in implementation of holistic care.
These challenges emphasize the need for a dermatologist‐guided skin care routine to improve patient confidence and reduce confusion over product selection. The panel advocates a patient‐centric approach based on patient factors and preferences focusing on education and practical recommendations on appropriate use of cleansers, moisturizers, and sunscreens. Readily available patient educational material, practical instructions, and staff training are recommended for improving patient and physician awareness on holistic skin care routines.,
With the plethora of products available on the market, it is not easy for physicians to verify the truthfulness of product claims, such as hypoallergenic, non‐irritating, non‐allergenic, non‐comedogenic, and non‐acnegenic. Physicians should be aware that such common claims are marketing tools with minimal regulatory validation. Physicians should look at proof of efficacy studies to validate claims such as skin hydration, transepidermal water loss, hypoallergenic, or UV protection. Physicians should consider the key ingredients and supporting scientific evidence before prescribing skin care products. For example, benzoyl peroxide in strengths of up to 10% and salicylic acid in strengths of up to 2% are FDA approved ingredients in OTC acne products. With reference to cosmetics, physicians should be cognizant with the term “alcohol‐free” products, because alcohol‐free refers to the solvent ethyl alcohol, which can cause skin dryness. However, alcohol‐free products can also contain “fatty alcohols” such as cetyl, stearyl, cetearyl, or lanolin alcohol, which can be confusing in an alcohol‐free product claim. On the contrary, fatty alcohols are skin friendly as they help to retain moisture. In context with therapeutic moisturizers, as per the US FDA over‐the‐counter monographs, only products containing hydrocortisone or colloidal oatmeal can claim to provide eczema relief. It is noteworthy that the regulation of ingredients and claims in cosmetics vary across countries. For instance, benzoyl peroxide is not allowed to be listed as a cosmetic ingredient in certain areas, while products containing colloidal oatmeal cannot claim to provide eczema relief in some others, thus requiring individualized consideration. The consensus panel, therefore, emphasizes the role of dermatologist guided CMP routine to reduce patient confusion over unsubstantiated product claims.
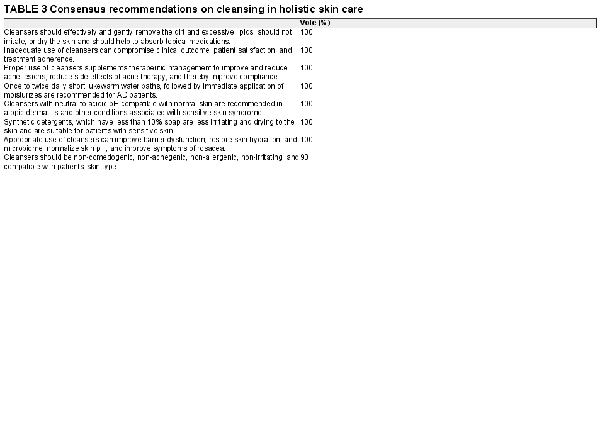
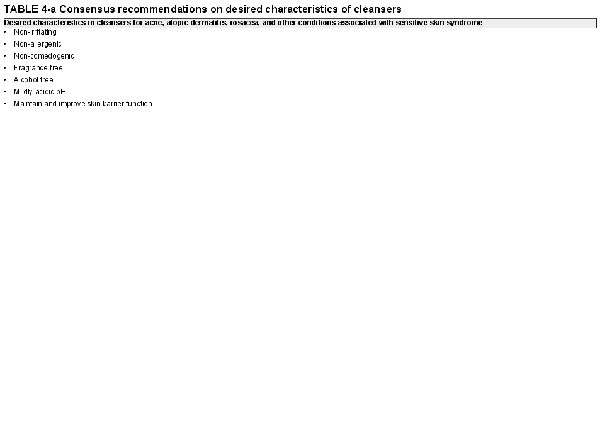
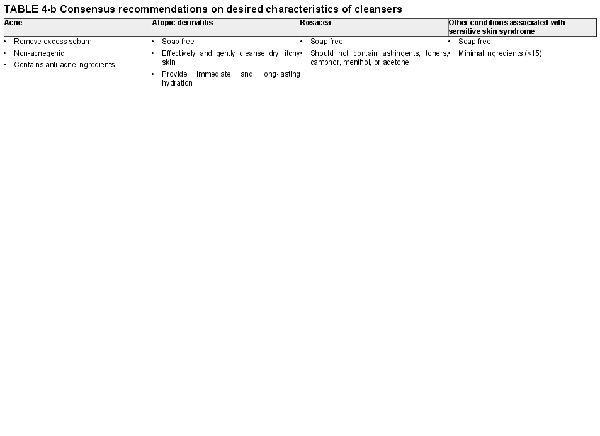
4.2 Consensus recommendations on cleansing
Cleansing (C) forms a vital component of holistic skin care. Studies have documented beneficial effects of cleansing in acne with removal of sebum leading to reduction in both inflammatory and non‐inflammatory acne lesions. The panel recommends that cleansers for acne should be non‐irritating, non‐allergenic, non‐comedogenic, non‐acnegenic and alcohol‐free while also removing excess sebum. Cleansing frequency recommendation varies across countries mainly depending on climatic conditions. In hot, tropical climates cleansing is recommended up to three times a day, while in dry, winter climates twice daily cleansing is sufficient. The panel advises against excessive cleansing as it can lead to skin dryness and irritation, which can adversely affect topical therapy compliance and clinical outcomes.
Highlighting the benefits of cleansing in atopic dermatitis (AD), a randomized control trial, showed that body wash formulae with lipids and zinc pyrithione significantly reduced the colonization of staphylococcus aureus, improved microbial diversity, reduced corticosteroid consumption, and showed clinically important improvement from baseline in SCORAD (SCORing Atopic Dermatitis) at the end of 4 weeks. Because cleansers with alkaline pH can strip proteins, lipids, and natural moisturizing factors off the stratum corneum, the panel recommends non‐soap cleansers with neutral to acidic pH, hydrating cleansers that leave a film of moisturizer over the skin surface and short, lukewarm baths for AD patients.
The benefits of cleanser and moisturizer regimen have also been demonstrated in the Assessment of Skin Characteristics Study, a multicenter open‐label study, which showed reduced severity and duration of stinging, burning, tingling, and itching in rosacea. Patients with rosacea have sensitive skin, and since detergents containing sodium lauryl sulfate can cause skin irritation, soap‐free cleansers are recommended. Synthetic detergents (syndets) are preferred because they are soap free and their pH is compatible with natural skin. To avoid any potential irritants, cleansers for rosacea and other sensitive skin disorders should be alcohol free and should contain minimal mild surfactants. Products containing astringents, tonics, camphor, or menthol should be avoided. Fragrance free cleansers are preferred as they reduce the risk of sensitization and contact allergy.
Properties such as alcohol‐free, soap‐free, and sodium lauryl sulfate‐free should not be considered by all‐or‐none manner. Different ingredient concentration and formulation could lead to different product property. Although alcohol is added to skin care products to make the product feel light, allow better absorption of ingredients or as a preservative, alcohol can disrupt the skin barrier and cause skin dryness. Consequently, alcohol‐free cleansers are preferred in those predisposed to skin dryness. Depending on their molecular charge, surfactants in cleansers are either anionic, cationic, amphoteric, or non‐ionic. Anionic surfactant like sodium lauryl sulfate (SLS) is a common ingredient in cleansers because of its foaming and lathering characteristics. However, the irritation potential of each surfactant is different. For example, both SLS and sodium cocoyl isethionate (SCI) are anionic surfactants, but SLS causes significant skin irritation. Combining sodium laureth sulfate (SLES) (anionic surfactant closely related to SLS) with amphoteric surfactants results in a milder cleanser formula with reduced skin irritation. The consensus recommendations on cleansing and desired characteristics of cleansers are summarized in Tables 3 and 4.
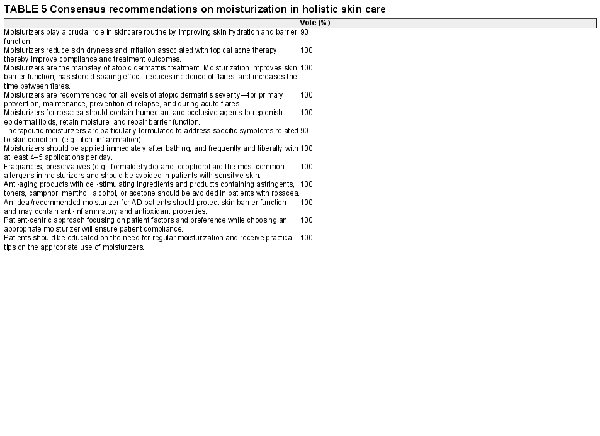
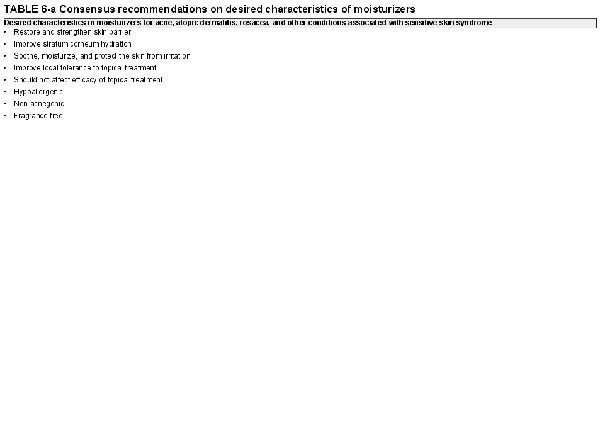
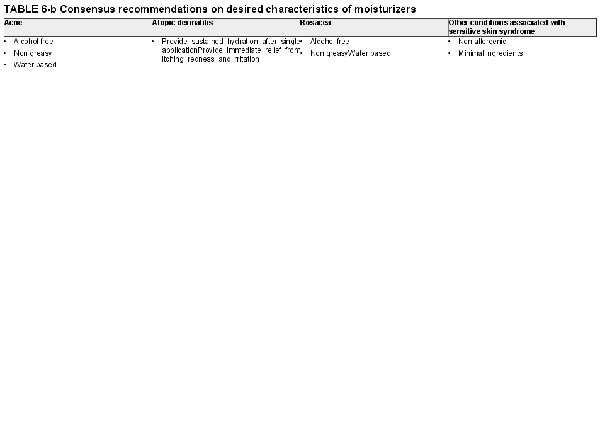
4.3 Consensus recommendations on moisturization
Moisturization plays a crucial role in holistic skin care by improving skin hydration and barrier function, the recommendations for which are summarized in Table 5. Clinical evidence in AD demonstrates the efficacy of moisturizers in reducing symptoms (e.g., pruritus, erythema, and fissuring) and requirement of anti‐inflammatory treatment. In a Cochrane pooled analysis of six studies, daily moisturization significantly reduced the number of flares, increased the time to flare, and reduced the use of topical corticosteroids as compared with untreated controls. By reducing the number of flares, moisturizers can improve quality of life, reduce sick days at work, and thus provide potential cost benefit. The panel recommends liberal and frequent application of moisturizer at least 2–3 times daily and immediately after shower in AD patients. (Table 6) Moisturizers used in AD should provide sustained hydration after single application, as well as soothe, moisturize, and protect the skin from irritation. Moisturizers should restore and strengthen skin barrier and provide immediate relief from itching, redness, and irritation. Additionally, moisturizers should be easy to apply to the skin, should not leave a greasy film, and should not stain clothing. The type of moisturizer recommended should be based on patient preference to ensure compliance. Moisturizers with known irritants, and sensitizers should be avoided.
It should be noted that all moisturizers are not equal. Emollients (e.g., Vaseline) provide lubrication and skin softening, occlusive ingredients (e.g., liquid paraffin) provide barrier protection and reduce water loss, while humectants (e.g., glycerine) attract and bind water. Therapeutic moisturizers are particularly formulated with ingredients that counter specific symptoms such as itch (e.g., colloidal oatmeal) and inflammation (e.g., hydrocortisone) or target underlying barrier disruption or ceramide deficiency (e.g., ceramides and urea). Prescription emollient devices (PED) are topical agents (anti‐inflammatory, humectants, or emollients) used in atopic dermatitis to target defects in skin barrier function through physically mediated effects. PEDs are FDA approved as 510(k) medical devices based on their ability to demonstrate equivalence to already existing barrier creams.
Moisturizers are crucial in improving treatment adherence by mitigating skin dryness and irritation, which are the common side effects of acne therapy., In mild–moderate acne, a regimen of cleanser and an active formulation moisturizer reduced the mean total lesion count (6.9% vs. 1.4%), pustular lesions (p < 0.05), and sebum levels (p < 0.01) and reduced colonization of Propionibacterium acne (49.4% vs. 3.2%) compared to vehicle. However, it is essential to note that acne therapies such as benzoyl peroxide and retinoids can affect epidermal barrier function and may cause skin irritation specifically during initial application. Therefore, water‐based moisturizers are preferred in acne as indicated in Table 6. The panel advises that moisturizers for acne should improve stratum corneum water content, should not affect the efficacy of topical acne treatment, and should improve tolerance to topical treatment. Additionally, hypoallergenic, alcohol‐free, and water‐based moisturizers are recommended.
In another study a skin care regimen of redness control moisturizing cream, night repair cream, and facial wash reduced transepidermal water loss (TEWL) (p < 0.001) and increased skin hydration (p < 0.001) in patients with rosacea. Similarly, Hawkins et al demonstrated the benefits of a mild cleanser and moisturizer regimen in patients with self‐perceived sensitive skin and dermatologist‐assessed sensitive skin (with rosacea and AD). A significant reduction in dermatologist‐assessed dryness, erythema, and severity of skin condition was noted with increased skin smoothness, softness, and overall appearance.
The panel recommends that moisturizers should be hypoallergenic, alcohol‐free, water‐based, and non‐greasy, to avoid irritation of the sensitive skin. (Table 6) Water‐based products have water as the main ingredient, feel light on the skin and offer a cooling effect due to water evaporation from the skin surface. Non‐greasy products are beneficial as they do not leave greasy films after application and are less occlusive. For sensitive skin, moisturizers with hydrophilic formulations and low lipid content are preferred because those with high lipid content such as mineral oils can lead to heat accumulation and worsen some skin conditions. Moisturizers for sensitive skin syndrome should restore barrier function and reduce water loss. Moisturizers with hydrating agents that retain water (glycerine, hyaluronic acid, or ceramides) are beneficial while the use of products containing irritants (e.g., benzoic acid, sodium lauryl sulfate) should be minimized in sensitive skin syndrome. The panel highlights the unmet need for moisturizers with active ingredients to address the underlying pathogenesis of sensitive skin syndrome.
4.4 Consensus recommendations on photoprotection
Photoprotection (P) constitutes the third important component of holistic skin care. Ultraviolet (UV) radiation is known to affect skin barrier function, trigger skin inflammation, and aggravate atopic dermatitis and rosacea. UV radiation can also increase the thickness of the stratum corneum and cause microbial dysbiosis and thus aggravate acne flares. Furthermore, some topical and systemic acne therapies can increase the risks of phototoxicity. Physicians should therefore educate patients on avoidance of midday sun and use of protective clothing as the first essential steps for photoprotection along with use of sunscreens.
Because the use of photoprotective moisturizer has demonstrated reduced skin irritation and improved tolerability of topical medication in acne patients, the panel recommends use of broad spectrum (UVA/UVB) SPF ≥30 sunscreen to reduce acne therapy‐induced photosensitivity and photodermatitis, as summarized in Table 7. Photoprotection, including protection from visible lights is particularly essential in Asian patients because Asian skin (mainly Fitzpatrick skin type IV and V) is more prone to post‐inflammatory hyperpigmentation. Sunscreen should be prescribed as early as possible, notably in young patients, to develop good skincare habits. Since Asian skin may react differently to topical agents, dermatologists should consider differences between Asian and Caucasian skin when prescribing sunscreens.
In patients with sensitive skin due to underlying acne, atopic dermatitis or rosacea, and idiopathic sensitive skin syndrome, sunscreen selection needs careful consideration to avoid potential irritants and allergens. Patients should be asked about previous intolerance, irritant, or allergic experience. Inorganic UV filters (titanium dioxide and zinc oxide), also known as physical filters, have lower allergenic potential and are therefore preferred in sensitive skin conditions. Sunscreen should not be applied over inflamed skin to prevent systemic absorption and photosensitization, an unmet need for sunscreens that can be applied over inflamed skin is identified. The panel recommends broad‐spectrum (UVA/UVB) sunscreen with SPF 30 for atopic dermatitis and rosacea. (Table 7).
5 CONCLUSION
Conditions such as acne, rosacea, and atopic dermatitis have underlying differences in pathogenesis and treatment, thus requiring individualized treatment and personalized skin care. While treatment is a definitive therapeutic component in the management of these conditions, adjunctive treatment is just as important in alleviating symptoms and signs of the disease, reducing the use of therapeutic agents and their side effects and improving the quality of life. It is crucial to initiate therapeutic treatment first and consider individual skin differences and understand product details to include cleansing, moisturization, and photoprotection (CMP) in accordance with different stages of disease course. The consensus recommendations presented here provide practical guidance on role of CMP in holistic care to achieve overall better patient compliance, satisfaction, and treatment outcomes.
AUTHOR CONTRIBUTIONS
The authors confirmed contribution to the paper as follows: All authors had participated in an online survey, and had attended the expert meeting conducted online, held on March 4, 2022, the discussion of which formed the basis of this manuscript. All authors have made substantial contributions to conception and design, acquisition of data, and analysis and interpretation of data. CL Goh has been involved in drafting the manuscript or revising it critically for important intellectual content. All authors had reviewed the results, read and approved the final version of the manuscript and agreed to be accountable for all aspects of the work. None of the authors received any honorarium for the preparation of the manuscript.
CONFLICT OF INTEREST
All authors have served as consultants for Galderma as advisory board members. CL Goh is a consultant to Neoasia (Singapore) and has served on advisory boards for Cantabria Lab (Spain), Galderma, and LaRoche Posay. B Welsh received honorarium for consultancy work for Galderma, Eli Lilly, Sanofi Aventis, AbbVie, Janssen‐Cilag, and Candela. M F Abad‐Casintahan is a consultant Dermatologist and Medical Director for Galderma, Philippines. The other authors have nothing to disclose.
ETHICAL APPROVAL
Authors declare human ethics approval was not needed for this study.
ACKNOWLEDGMENT
This paper was compiled based on discussions during an online expert meeting convened on March 4, 2022, attended by all authors and sponsored by Galderma Singapore. The content reflects the opinion of the authors. None of the authors received any honorarium for the preparation of the manuscript. The authors wished to acknowledge Dr Sheila Chua, Head of Medical Affairs, Galderma Japan, and Asia Pacific region, and Dr Vaijayanti Karandikar and See Mee Yen of Medica Comms, for assistance with the preparation of this publication.
REFERENCES
- 1. Del Rosso JQ, Gold M, Rueda MJ, Brandt S, Winkelman WJ. Efficacy, safety, and subject satisfaction of a specified skin care regimen to cleanse, medicate, moisturize, and protect the skin of patients under treatment for acne vulgaris. J Clin Aesthet Dermatol. 2015;8(1):22–30.
- 2. Lee YB, Shin MK, Kim JS, et al. Perceptions and behavior regarding skin health and skin care products: analysis of the questionnaires for the visitors of skin health expo 2018. Ann Dermatol. 2020;32(5):375–382.
- 3. Goh CL, Noppakun N, Micali G, et al. Meeting the challenges of acne treatment in Asian patients: a review of the role of Dermocosmetics as adjunctive therapy. J Cutan Aesthet Surg. 2016;9(2):85–92.
- 4. Higham R. Integration of moisturizers and cleansers into a busy dermatology practice. Cutis. 2005;76(6 Suppl):32–33.
- 5. Berson D. Recommendation of moisturizers and cleansers: a study of unmet needs among dermatology patients. Cutis. 2005;76(6 Suppl):3–6.
- 6. Misery L, Ständer S, Szepietowski JC, et al. Definition of sensitive skin: an expert position paper from the special interest group on sensitive skin of the international forum for the study of itch. Acta Derm Venereol. 2017;97(1):4–6. doi:10.2340/00015555-2397
- 7. Guerra‐Tapia A, Serra‐Baldrich E, Prieto Cabezas L, González‐Guerra E, López‐Estebaranz JL. Diagnosis and treatment of sensitive skin syndrome: an algorithm for clinical practice. Actas Dermosifiliogr. 2019;110(10):800–808.
- 8. Maher TM, Whyte MK, Hoyles RK, et al. Development of a consensus statement for the definition, diagnosis, and treatment of acute exacerbations of idiopathic pulmonary fibrosis using the Delphi technique. Adv Ther. 2015;32(10):929–943. doi:10.1007/s12325-015-0249-6
- 9. Nicol NH. Use of moisturizers in dermatologic disease: the role of healthcare providers in optimizing treatment outcomes. Cutis. 2005;76(6 Suppl):26–31.
- 10. Xu S, Kwa M, Lohman ME, Evers‐Meltzer R, Silverberg JI. Consumer preferences, product characteristics, and potentially allergenic ingredients in best‐selling moisturizers. JAMA Dermatol. 2017;153(11):1099–1105.
- 11.
- 12. Hebert AA, Rippke F, Weber TM, Nicol NH. Efficacy of nonprescription moisturizers for atopic dermatitis: an updated review of clinical evidence. Am J Clin Dermatol. 2020;21(5):641–655. doi:10.1007/s40257-020-00529-9
- 13. Andriessen A, Jiang X, Kulthanan K, Lee CH, Sinclair R, Zhang CF. Recommendations for using over‐the‐counter products as adjunctive acne Care in Asian Phototypes: improving treatment outcomes and managing side effects. J Drugs Dermatol. 2021;20(11):1213–1221. doi:10.36849/jdd.6259
- 14. Xu Z, Liu X, Niu Y, et al. Skin benefits of moisturising body wash formulas for children with atopic dermatitis: a randomised controlled clinical study in China. Australas J Dermatol. 2020;61(1):e54–e59. doi:10.1111/ajd.13153
- 15. Levin J, Miller R. A guide to the ingredients and potential benefits of over‐the‐counter cleansers and moisturizers for rosacea patients. J Clin Aesthet Dermatol. 2011;4(8):31–49.
- 16. Del Rosso JQ. The use of moisturizers as an integral component of topical therapy for rosacea: clinical results based on the assessment of skin characteristics study. Cutis. 2009;84(2):72–76.
- 17. Kresken J, Wigger‐Alberti W, Clanner‐Engelshofen BM, Reinholz M. Dermocosmetics for use in rosacea: guideline of the society for Dermopharmacy. Skin Pharmacol Physiol. 2018;31(3):147–154.
- 18. Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. Diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70(2):338–351. doi:10.1016/j.jaad.20
- 19. van Zuuren EJ, Fedorowicz Z, Christensen R, Lavrijsen A, Arents BWM. Emollients and moisturisers for eczema. Cochrane Database Syst Rev. 2017;2(2):CD012119. doi:10.1002/14651858.CD012119.pub2
- 20. Matsunaga K, Leow YH, Chan R, Kerrouche N, Paliargues F. Adjunctive usage of a non‐comedogenic moisturizer with adapalene gel 0.1% improves local tolerance: a randomized, investigator‐blinded, split‐face study in healthy Asian subjects. J Dermatolog Treat. 2013;24(4):278–282. doi:10.3109/09546634.2012.661037
- 21. Hayashi N, Kawashima M. Study of the usefulness of moisturizers on adherence of acne patients treated with adapalene. J Dermatol. 2014;41(7):592–597. doi:10.1111/1346-8138.12520
- 22. Angelova‐Fischer I, Rippke F, Fischer TW, Neufang G, Zillikens D. A double‐blind, randomized, vehicle‐controlled efficacy assessment study of a skin care formulation for improvement of mild to moderately severe acne. J Eur Acad Dermatol Venereol. 2013;27(Suppl 2):6–11. doi:10.1111/jdv.12168
- 23. Del Rosso JQ. The role of skin care as an integral component in the management of acne vulgaris: part 1: the importance of cleanser and moisturizer ingredients, design, and product selection. J Clin Aesthet Dermatol. 2013;6(12):19–27.
- 24. Santoro F, Lachmann N. An open‐label, intra‐individual study to evaluate a regimen of three cosmetic products combined with medical treatment of rosacea: cutaneous tolerability and effect on hydration. Dermatol Ther (Heidelb). 2019;9(4):775–784. doi:10.1007/s13555-019-00331-4
- 25. Hawkins SS, Subramanyan K, Liu D, Bryk M. Cleansing, moisturizing, and sun‐protection regimens for normal skin, self‐perceived sensitive skin, and dermatologist‐assessed sensitive skin. Dermatol Ther. 2004;17(Suppl 1):63–68. doi:10.1111/j.1396-0296.2004.04s1008.x
- 26. Passeron T, Lim HW, Goh CL, et al. Photoprotection according to skin phototype and dermatoses: practical recommendations from an expert panel. J Eur Acad Dermatol Venereol. 2021;35(7):1460–1469. doi:10.1111/jdv.17242