Introduction
The extra-alveolar sites for the placement of mini-implant are selected depending on the biomechanics to be used and the quality of bone present at the site of placement. At present, the mandibular buccal shelf (MBS) area is used for mini-screw insertion mainly for the correction of class III problems and correction of severe skeletal and dental malocclusions without extractions or extensive surgical procedures. There are a gamut of variations when it comes to selecting the site of implant placement in the buccal shelf area because of varying mandibular anatomy. Thus, with the assumption that mandibular anatomy varies in patients with different facial divergence, the site and angulation of buccal shelf implant placement also differs as per the anatomy. Henceforth, it is important to determine the cortical bone thickness of the buccal shelf area and the site of buccal shelf implant placement in individuals with different facial divergence. Moreover, authors suggest that placing the mini-implant at an angle to the bone surface increases the bone contact. Studies also suggest that to distalize the entire mandibular arch, the mini-screw should be placed at an angle perpendicular to the occlusal plane.,
The purpose of this study was to record measurements from cone beam computed tomography scans to quantify the cortical bone thickness of MBS region and find out the preferable site for buccal shelf implant placement in 10 hyperdivergent and 10 hypodivergent patients. The study gauges MBS relative to:
The angle of slope, which is measured between the outer cortical outline of the buccal shelf area and the long axis of the respective molar
The cortical bone thickness which is measured at 90° to the outer buccal cortex
The amount of cortical bone engagement when the screw is placed lateral to the molar roots, approximately perpendicular to the occlusal plane, ie, 30° angle to the outer buccal cortex.
Material and Methods
Sampling
Purposive sampling was done retrospectively by collecting 20 pretreatment cone beam computed tomography scans of adult patients with the age range of 19 to 25 years (10 hypodivergent and 10 hyperdivergent) from the preexisting college records.
Inclusion criteria: All the included subjects were of Indian origin. Subjects who have not undergone orthodontic or orthopedic intervention were included. Groups were classified based on the Frankfort mandibular plane angle (FMA < 22° were included in hypodivergent group whereas FMA > 27° were included in hyperdivergent group), ascending ramus, mandibular base length, Jarabak ratio and Downs Y-axis, and subjects with healthy periodontium and adequate alveolar bone support were included in the study (alveolar crest 1.5–2 mm apical to cementoenamel junction).
Exclusion criteria: Patients with gross facial asymmetries, prosthesis on molars, and missing teeth at the site of examination were not included. Also, patients with bone metabolic and systemic diseases were not included.
Measurements Recorded
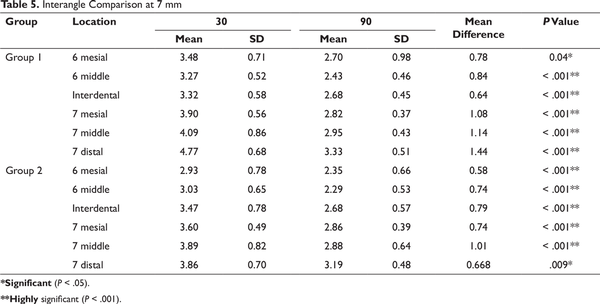
6 sites were examined on the right side of mandible (as there is bilateral symmetry): mesial of first molar (6M), middle of first molar (6Mi), interdental between the first and second molar (Id), mesial of the second molar (7M), middle of the second molar (7Mi), and distal of the second molar (7D; Figure 1). The subsequent bone measurements were carried out on coronal section and curved slicing in cone beam computed tomography scans at the above mentioned 6 sites. The alveolar crest was the horizontal baseline.
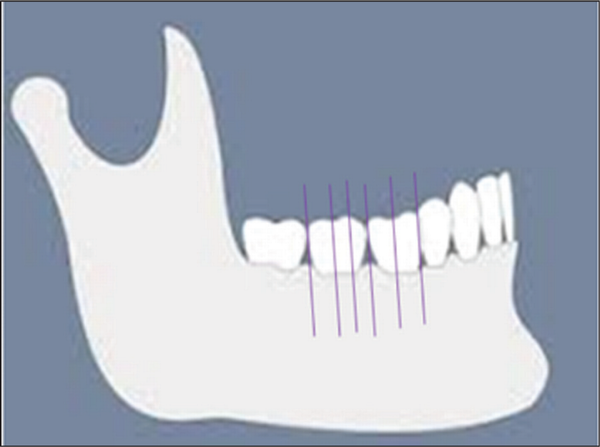
The angle of slope was measured between the cortical outline of the buccal shelf area and the long axis of the respective molar (Figure 2a).
The cortical bone thickness was measured at 90° and 30° angle as shown at 3, 5, and 7 mm from the alveolar bone crest (Figure 2a,b,c).
Bone engagement depth of an 8-mm mini-implant is 3 mm, of a 10-mm bone screw is 5 mm, and of a 12-mm bone screw is 7 mm; and therefore, 3, 5, and 7 mm measurements were selected from the alveolar crest.
All the collected data were analyzed on the Carestream dental (CS 3D [Carestream dental, Rochester, NY, USA]) imaging software.
Sites Examined Are Marked with Purple Lines
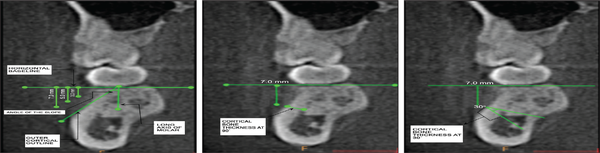
Figure 2
(a) 3, 5, and 7 mm Vertically Down From the Alveolar Crest and Angle of the Slope of the Mandibular Buccal Shelf (b) Measurement of Cortical Bone Thickness at 90° to the Outer Buccal Cortex and 7 mm Vertically Down From the Alveolar Crest (c) Measurement of Cortical Bone Thickness at 30° Angulation and 7 mm Vertically Down From the Alveolar Crest.
Results
Data were analyzed using SPSS version 23. Descriptives, one-way analysis of variance for intragroup comparison, independent t-test for intergroup comparison, paired t-test for interangle (30° and 90°) comparison, and P ≤ .05 was considered significant.
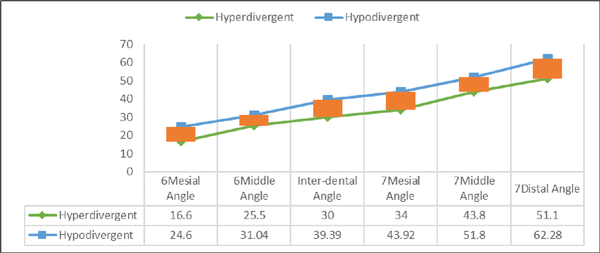
A significant change in anatomy was seen at the angle of buccal shelf slope at the mesial of first molar (P = .001), mesial of second molar (P = .008), distal of second molar (P = .003; Figure 3).
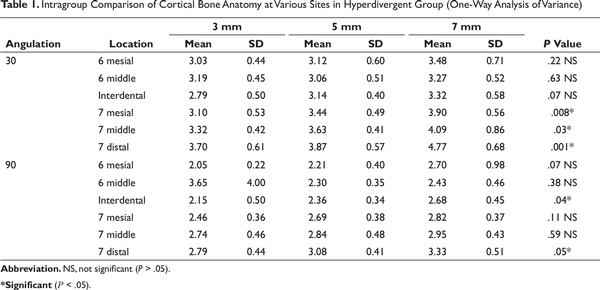
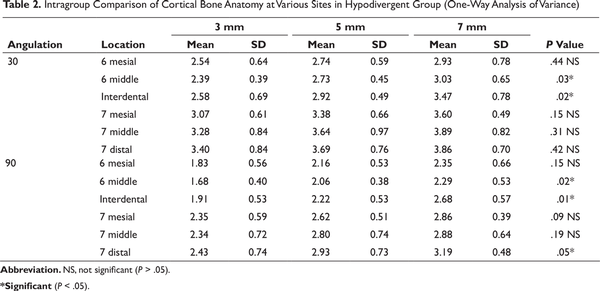
Intragroup comparison of cortical bone anatomy of MBS for hyperdivergent group showed statistically significant differences at 3, 5, and 7 mm from the alveolar crest. At 30° angulation, significant differences were noted at the mesial (P = .008), middle (P = .03), and distal (P = .001) of the mandibular second molar. At 90° angulation, a significant difference was present at the interdental (P = .04) between the first and the second molar and distal to the second molar (P = .05; Table 1). Intra-group comparison of cortical bone anatomy of MBS for hyperdivergent group showed statistically significant differences at various sites at 3, 5, and 7 mm from the alveolar crest (Table 2). The maximum mean amount of cortical bone for hypodivergent group distal to the second molar is 4.77 ± 0.68 mm at 30° angulation and for hypodivergent group is 3.86 ± 0.70 mm at 30° angulation, and at the middle of the second molar for hyperdivergent group this value is 4.09 ± 0.86 mm and for hypodivergent group it is 3.89 ± 0.82 mm at 30° angulations (Table 5).
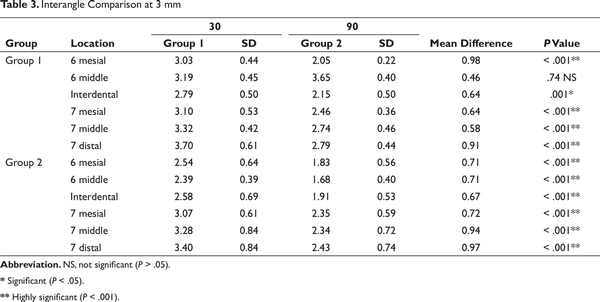
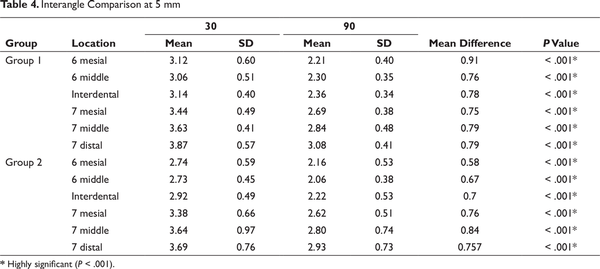
High statistically significant differences were noted at the insertion site at 90° and 30° angulations for both groups at 3, 5, and 7 mm at all sites (Tables 3, 4, 5). The mean difference in the amount of cortical bone at 90° and 30° placement 7 mm from the alveolar crest at the middle of mandibular second molar for hyperdivergent group is 1.14 mm and for hypodivergent group is 1.01 mm and at 90° and 30° placement at distal of mandibular second molar for hyperdivergent group is 1.44 mm and for hypodivergent group is 0.668 mm (Table 5).
Comparative Evaluation of Angular Measurements in Hyperdivergent and Hypodivergent Groups
Discussion
Newton’s third law of motion states: “For every action, there is an equal and opposite reaction.” This law is also applicable in orthodontics: for every desired tooth movement, there is a potential to create an undesired tooth movement. This was the problem when teeth were used as anchor units. Inspired by the stability of prosthodontic implants, orthodontists modified the use of these implants for absolute anchorage purpose.
These mini-screws provide absolute anchorage by absorbing the reactive forces and transmitting it to skeletal structures, thus the undesirable side effects can be prevented entirely. As they are anchored directly on the skeletal structures, no root to mini-implant contact occurs and hence no damage to the root happens. Also, a long range of action can be achieved. Owing to all these advantages, we can easily distalize the entire dentition and borderline surgical cases were converted into nonsurgical cases. Moreover, we can achieve a three-dimensional control on the applied orthodontic or orthopedic forces along with maintaining the integrity of both maxillary and mandibular arches.,
Facial divergence of an individual has an important role in determining the type of biomechanics to be used in orthodontics. There is always more anchorage requirement in individuals with hyperdivergent growth pattern as compared to hypodivergent growth pattern. The anatomy of the mandible, and thus the buccal shelf area, is different in hyperdivergent and hypodivergent growth patterns. It becomes mandatory to have adequate knowledge of anatomy as well as the amount of cortical bone available at the site of insertion of the bone screw.
Two popular sites of extra-alveolar placement of mini-screw are infra-zygomatic crest and buccal shelf area. Bone screws are manufactured of pure stainless steel., Bone screws are generally placed in areas of D1 ( > 1250 HU) quality bone and therefore require greater fracture resistance. Stainless steel provides greater fracture resistance than titanium alloy and, therefore, it is the material of choice.
This study focuses on the facial divergence pattern of an individual, as the anatomy of the mandible is different in patients of different facial divergence because of the muscle forces. It was interesting for us to find out the difference in the anatomy of the buccal shelf area, the site of implant placement, and the buccal cortical bone thickness for these 2 groups.
Power analysis was performed with the GPower 3.1 software for the sample size selection. (Effect size = 0.282, α = 0.05), (1-β) = 0.80, and (N2/N1 = 1)
In the present study, 6 sites were examined: mesial of the first molar, middle of the first molar, interdental between the first and second molar, mesial of the second molar, middle of the second molar, and distal of the second molar.
Angular measurements of the slope of buccal shelf area to the respective molar show broader buccal shelf area in hypodivergent group (increased angular measurements) as compared to hyperdivergent group. A significant change in anatomy was seen at the angle of buccal shelf slope at mesial of first molar (P = .001), second molar mesial (P = .008), second molar distal (P = .003; Figure 3). Thus, an interesting finding is that in hypodivergent individuals, because of broader buccal shelf area, the screw can be placed farther from the dentition compared to the hyperdivergent individuals.
The results obtained suggest that the favorable site of buccal shelf implant placement is distal to the second molar which correlates with the study of Baumgaertel. Similar study carried out by Liu et al at Guangzhou Medical University concluded that the ideal site for buccal shelf implant placement is between distobuccal of first molar and mesiobuccal of the second molar. The growth pattern of an individual was not considered in this study. The present study accounts for the facial divergence, and the site for buccal shelf implant placement between distobuccal of the first molar and mesiobuccal of the second molar is suitable when the screw is placed at an obtuse degree angulation. A significant finding of our study is that the amount of cortical bone available is more when the buccal screw is inserted at 30° to the occlusal plane which is in accordance with the study of Chang et al. We found high statistically significant differences in the angulation of bone placement distal to the second molar for both the hyperdivergent and hypodivergent groups.
The anatomy of the mandible, and thus the buccal shelf area, is different in hyperdivergent and hypodivergent growth patterns. The hyperdivergent group has flat mandibular anatomy and hence a narrow buccal shelf area when compared to the hypodivergent group. Mean amount of cortical bone when the screw is placed at 30° for hyperdivergent group distal to the second molar is 4.77 ± 0.68 mm and for hypodivergent group is 3.86 ± 0.70 mm. Another statistically significant site for implant placement is middle of mandibular second molar at 30° where the mean amount of cortical bone for hyperdivergent group is 4.09 ± 0.86 mm and for hypodivergent group is 3.89 ± 0.82 mm.
Thus, a good amount of cortical bone is available at both 90° and 30° angulations for both the groups, when the screw is placed distal to the mandibular molar. However, comparatively more bone is available at 30° angulated placements. The difference in the mean cortical bone at 90° and 30° is more in hyperdivergent group than in hypodivergent group. Whereas, for the middle of the second molar only 30° angulated placements are favorable for both groups.
When a mini-implant is placed distal to mandibular second molar, the proximity of nerve should be examined. According to the study of Elshebiny et al, the distance between the nerve and mini-implant placed distal to mandibular second molar is safe enough for the placement without damaging the nerve.
The thickness of the soft tissue affects the stability of mini-screw. This study was focused on the bony architecture of the buccal shelf area and soft tissue parameters were not taken into consideration.
Conclusion
The optimal site for buccal shelf implant placement is distal to the mandibular second molar. Another suitable site is middle of mandibular second molar at an obtuse angulation of placement.
Hyperdivergent individuals have narrow buccal shelf area compared to the hypodivergent individuals.
The maximum amount of cortical bone was found distal to the second molar at 7 mm vertically from alveolar crest when the implant was placed at 30° angulation for both the groups. The difference in the cortical bone thickness at 90° and 30° is more in hyperdivergent group than hypodivergent group.
Bharvi K Jani
https://orcid.org/0000-0001-6456-2457
- 1. Chang C, Huang C, Roberts WE. 3D cortical bone anatomy of the mandibular buccal shelf: a CBCT study to define sites for extra-alveolar bone screws to treat class III malocclusion. Int J Orthod Implantol. 2016; 41:74–82.
- 2. Inaba M. Evaluation of primary stability of inclined orthodontic mini-implants. J Oral Sci. 2009;51(3):347–353.
- 3. Park HS, Jeong SH, Kwon OW. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2006;130(1):18–25.
- 4. Newton I. Philosophiae Naturalis Principia Mathematica. London: Royal Society; 1687.
- 5. Roberts WE, Smith RK, Zilberman Y, Mozsary PG, Smith RS. Osseous adaptation to continuous loading of rigid endosseous implants. Am J Orthod. 1984; 86:95–111.
- 6. Chang CH, Liu SS, Roberts WE. Primary failure rate for 1680 extra-alveolar mandibular buccal shelf mini-screws placed in movable mucosa or attached gingiva. Angle Orthod. 2015;85(6):905–910.
- 7. Motoyoshi M, Matsuoka M, Shimizu N. Application of orthodontic mini-implants in adolescents. Int J Oral Maxillofac Surg. 2007;36(8):695–699.
- 8. Lin JJ. Treatment of severe class III with buccal shelf mini-screws. News Trend Orthod. 2010; 18:4–13.
- 9. Jong Lin JL. Textbook of Creative Orthodontics: Blending the Damon System and TADs to Manage Difficult Malocclusions. Taipei, Taiwan: Yong Chieh; 2007.
- 10. Ghosh A. Infra-zygomatic crest and buccal shelf - Orthodontic bone screws: a leap ahead of micro-implants, clinical perspectives. J Indian Orthod Soc. 2018;52:S127–S141.
- 11. Holmes PB, Wolf BJ, Zhou J. A CBCT atlas of buccal cortical bone thickness in inter radicular spaces. Angle Orthod. 2015;85(6):911–919.
- 12. Baumgaertel S. Planning and placing temporary anchorage devices (TAD’s) with the aid of cone beam computed tomography imaging. In: Kapila S ed. Cone Beamed Computed Tomography in Orthodontics: Indication Insight and Innovation. Hoboken: Wiley Blackwell; 2014:411–426.
- 13. Liu H, Wu X, Tan J, Li X. Safe regions of miniscrew implantation for distalization of mandibular dentition with CBCT. Prog Orthod. 2019;20:45.
- 14. Lascala CA, Panella J, Marques MM. Analysis of the accuracy of the linear measurements obtained by cone-beam computerized tomography. Dentomaxillofac Radiol. 2004; 33:291–294.
- 15. Elshebiny T, Palomo JM, Baumgaertel S. Anatomic assessment of the mandibular buccal shelf for miniscrew insertion in white patients. Am J Orthod Dentofacial Orthop. 2018; 153:505–511.