Introduction
Class II malocclusions often reflect imbalance or disharmony in maxilla-mandible, typically with the underdevelopment of the mandible and/or overdevelopment of the maxilla, leading to a convex soft tissue profile. According to Dr James McNamara, mandibular retrusion is the most common feature of Class II, Division 1 malocclusion in growing children. Ideally, treatment of Class II malocclusions should focus first on improving the skeletal discrepancy using functional appliances while the individual is still growing. The use of functional jaw orthopedics, at the correct time during growth, can ultimately result in achieving a broad beautiful smile, an excellent functional occlusion, a full face with a beautiful jaw line, and lateral profile.-
This article presents a case report of a young, growing female patient with mandibular retrognathism. Treatment was planned in 2 stages with the use of a twin-block appliance during the first phase to achieve forward positioning of the mandible for the correction of skeletal malocclusion, followed by the fixed orthodontic phase for camouflaging the remaining skeletal discrepancy and achieving a stable harmonious occlusion.
Case Report
Section I. Pretreatment Assessment: History and Clinical Examination (Figures 1 and 2)
PK, a 12-year-old female patient, came to the orthodontic department with a chief complaint of forwardly placed upper front teeth and clinically showed a Class II, Division 1 incisor relationship, on a skeletal Class II base, with the average maxillomandibular plane angle and the normal face-to-height ratio. She had a convex profile, incompetent lips, lip trap, deep mentolabial sulcus, lower lip eversion, and a clinically positive visual treatment objective. There was no relevant dental history.
Skeletal assessment: The patient showed no abnormal facial asymmetry and balance on frontal examination. She had a convex profile due to a Class II skeletal pattern, retrognathic mandible, average clinical Frankfort-mandibular plane, and normal proportions of lower anterior facial height.
Soft tissues: Both lips (upper and lower) were incompetent at rest with 6 mm of incompetency, a severe lip strain was observed upon forced closure. Concomitantly, lower lip eversion was seen with lip trap and a deep mentolabial sulcus, and a reduced nasolabial angle.
Clinical Examination: Intraoral Features (Figures 3 and 4)
General Dental Condition:
Maxillary arch:
U-shaped and asymmetrical arch form
Mild spacing in the anterior region
Proclined upper anteriors
Mandibular arch:
U-shaped and asymmetrical arch form
Lingually tipped 35
Uprighted anteriors
Occlusal features:
Incisor relationship: Class II, Division I
Overjet: 8 mm
Overbite: 4 mm
Center lines: Upper center line coincident with the facial midline. Lower center line displaced 1 mm to the left of the upper center line.
Left buccal segment relationship: Molar relation: Class II; canine relation: Class II
Right buccal segment relationship: Molar relation: Class II; canine relation: Class II
Crossbites: Scissor bite Irt 24, 25
Other occlusal features: Deep curve of Spee bilaterally
Diagnostic Summary
PK, a 12-year-old female patient, presented with a skeletal Class II due to orthognathic maxilla, retrognathic mandible, average growth pattern, Angle’s Class II, Division I malocclusion with Class II canine relation, mild anterior spacing, upper anterior proclination, uprighted lower anteriors, lingually tipped 35, increased overjet and overbite, scissor bite Irt 24, 25, acute nasolabial angle, tongue thrust habit, incompetent lips, and lower lip trap.
Buccal Segment Relationship
Full-cusp Class II, other occlusal features: Scissor bite (buccal nonocclusion) seen with upper-left first premolars with respect to the lower canines and premolars, and a deep curve of Spee bilaterally.
General Radiographic Examination (Figures 5A and B)
Pretreatment records obtained were panoramic a radiograph, a lateral cephalogram, and an MP3 radiograph for assessing the growth. The panoramic radiograph showed the presence of unerupted third molars with incomplete root formation in all the 4 quadrants. The radiographic examination showed the presence of restoration on upper first molars bilaterally. Normal alveolar bone levels and tooth root morphologies were noted. No supernumerary teeth, pathologic conditions, or abnormalities related to the condylar head or the temporomandibular joint space were found.
Cephalometric assessment revealed skeletal Class II jaw bases with an average growth pattern, average lower anterior facial height, and facial height ratio. Mild proclination of both maxillary and mandibular incisors, increased overbite and overjet, convex profile, and an acute nasolabial angle were also noted. Skeletal maturity using the cervical vertebral maturation index staging showed a Stage 2 of skeletal maturation (acceleration stage, with >65%–80% pubertal growth still remaining). The MP3 radiograph also showed 65% of growth remaining.
Model Analysis
Bolton’s analysis reveals mandibular tooth material excess in both overall and anterior regions.
Carey’s analysis suggested a discrepancy of 2 mm in the maxillary arch and 4 mm in the mandibular arch.
Aims and Objectives of Treatment
Correction of skeletal Class II malocclusion
Correction of axial inclination of upper incisors
Correction of molar relation
Correction of canine relation
Achieving ideal overjet and overbite
Correction of crowding, spacing, and scissor bite
Correction of tongue thrust habit
Treatment Plan
Treatment was carried out in the following 2 phases:
Extractions: Nonextraction
Phase I (Functional Phase): Orthopedic correction of the skeletal malocclusion with a standard twin-block appliance.
Phase II (Orthodontic Phase): Orthodontic correction and finishing and detailing with 0.22 slot MBT prescription brackets.
The orthodontic phase-included bonding both the upper and lower arches with a preadjusted edgewise appliance with an MBT (0.022 × 0.028 slot) prescription. As only minor dental corrections were required, anchorage consideration was not critical during this juncture. Therefore, only simple anchorage was utilized which was additionally reinforced by bonding the second molars. Supplemental dental treatment required in this case was oral prophylaxis.
Proposed Retention Strategy
For Phase I: Use of the fixed anterior inclined plane soldered to the upper molar bands during the orthodontic phase to maintain the mandibular advancement achieved.
For Phase II:
Upper arch: Upper Hawley’s retainer with the incorporated anterior inclined plane to be worn full time for 6 to 8 months followed by 12 hours use.
Lower arch: Lower Hawley’s retainer.
Section II: Treatment
After due deliberation with both patient and parents regarding the potential treatment plan, Phase I of the treatment was initiated. A standard twin-block appliance (Figure 4) was provided to the patient with a construction bite having an initial mandibular advancement of 8 mm. As the patient grew accustomed to using the appliance full time, appliance trimming was initiated subsequently. The functional phase took 6 months for completion (Figure 6).
After the conclusion of Phase I (Figures 7-9), a preadjusted edgewise appliance (using an MBT 0.022″ slot prescription) was bonded on both the upper and lower arches, and a 0.016″ NiTi was placed (Figure 10). A fixed lingual inclined plane was soldered to the first molar bands to maintain the mandibular advancement achieved during the functional phase and was in place till the occlusal settling was achieved. The second molars were banded to reinforce the anchorage after the alignment and leveling of the second molars, the occlusion was settled with vertical settling elastics. Phase II lasted for 12 months after which the fixed appliance was debonded (Figures 11-14) and the patient was given the upper and lower Hawley’s retainers (Figure 15). The upper Hawley’s retainer was incorporated with an anterior-inclined plane to maintain the skeletal correction achieved.
Leveling and Aligning
0.016 round NiTi upper and lower arches
0.016 × 0.022 rectangular NiTi upper and lower arches
0.017 × 0.025 rectangular SS upper and lower arches
0.019 × 0.025 rectangular SS upper and lower arches
0.021 × 0.025 rectangular SS upper and lower arches.
Finishing and Detailing
0.014″ SS archwire with settling elastics.
Prognosis for Stability
Provided that the lower incisors were not proclined excessively from their original position into the zone of influence of the lower lip, the general archform was maintained, and good occlusal interdigitation was achieved, and the long-term stability of treatment changes was considered good. In order to maximize the stability of skeletal correction, an anterior inclined plane was incorporated in the maxillary Hawley’s retainer.
Posttreatment Assessment
Occlusal Features
Incisor Relationship: Class I, Division I
Overjet: 2 mm
Overbite: 2 mm
Center lines: Coinciding
Left buccal segment relationship: Molar relation: Class I; canine relation: Class I
Right buccal segment relationship: Molar relation: Class I; canine relation: Class I
Crossbites: None
Displacements: None
Functional occlusal features: Mutually protected occlusion
Canine guidance: On the left and right lateral excursions with no working or nonworking side interferences
Anterior guidance: On protrusion with posterior disclusion.
Complications Encountered During the Treatment
No major complications were observed during the treatment. The patient was highly cooperative and used the appliance as recommended.
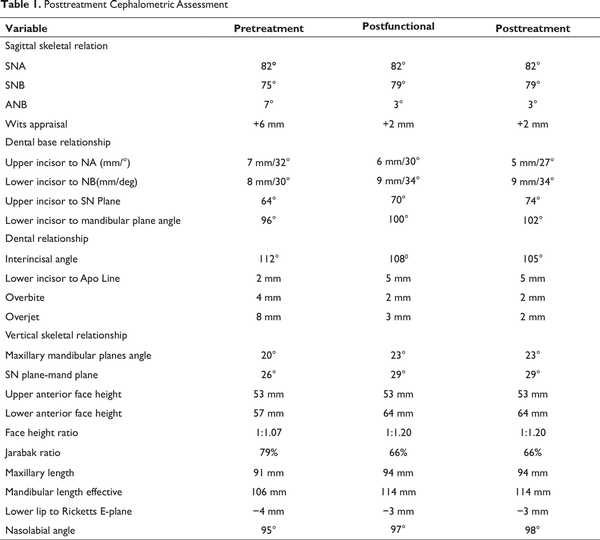
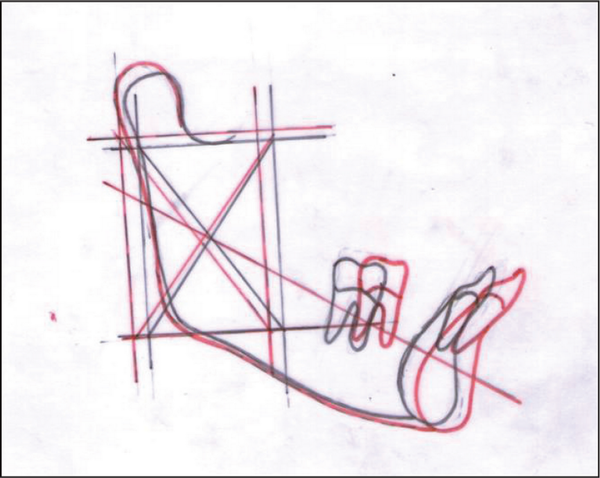
Posttreatment Cephalometric Assessment (Figures 14A, B, 16-19; Table 1)
Interpretation
Skeletal: The anteroposterior discrepancy of Class II skeletal base improved significantly following the functional phase and was maintained throughout the treatment. There was a significant increase of 4° in the SNB angle from 75° to 79°, and the Wits appraisal changed from 6 to 2 mm, which indicated the correction of skeletal Class II malocclusion. There was an increase of only 3 mm in the maxillary length due to the natural growth of the patient, whereas the mandibular body length increased by 8 mm from 106 to 114 mm due to the orthopedic correction. This improvement is demonstrated on the overall superimposition, with relatively more downward growth of the mandible than the maxilla. Average growth continued throughout treatment, as confirmed by the overall superimposition, and equated to a 7 mm increase in the total anterior face height. The maxillary-mandibular plane angle increased by 3° to 23°.
Dental: The upper incisor to maxillary plane angle decreased by 5° following correction of proclination and space closure in the upper labial segment. The lower incisor to mandibular plane angle increased by 6° to 102° suggesting mild proclination of the lower labial segment with treatment. As a result of these changes, the inter-incisal angle decreased to 105°. The lower incisal edge position retracted by 5 mm relative to A-Pogonion reference line shows mild proclination of the lower anteriors
Soft tissues: The nasiolabial angle increased by 4° and the lower lip position relative to Ricketts E-plane was reduced by 1 mm, both of which can be partly explained by the change in upper incisor position with treatment.

Pretreatment Extraoral Photographs

Visual Treatment Objective

Pretreatment Intraoral Photographs

Pretreatment Study Models
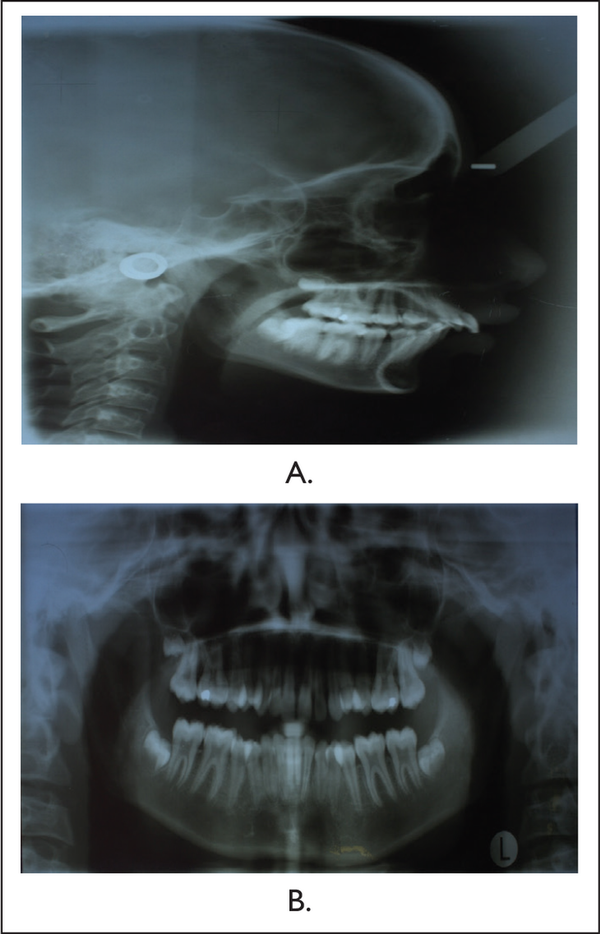
Pretreatment Radiographs: (A) Lateral Cephalogram and (B) Orthopantomogram

Twin-Block Appliance: Intraoral View

End of Functional Phase: Intraoral Photos

End of Functional Phase; Lateral Cephalogram
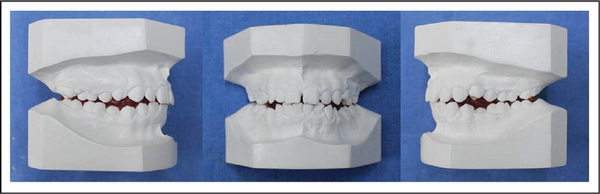
End of Functional Phase; Study Models

Bonding with 0022 MBT Brackets

Posttreatment Extraoral Photographs

Posttreatment Intraoral Photos

Posttreatment Models
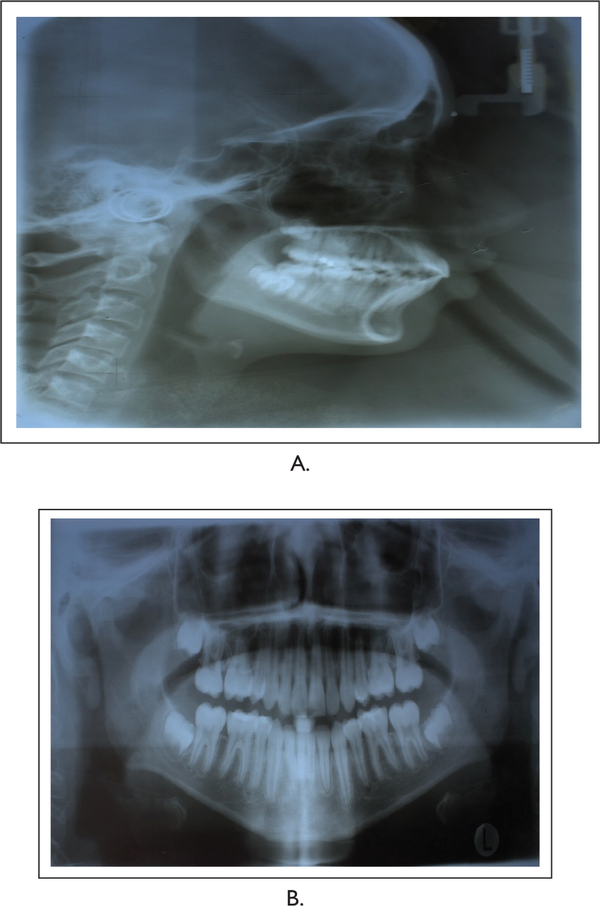
Posttreatment Radiographs: (A) Lateral Cephalogram and (B) Orthopantomogram

Posttreatment Retention
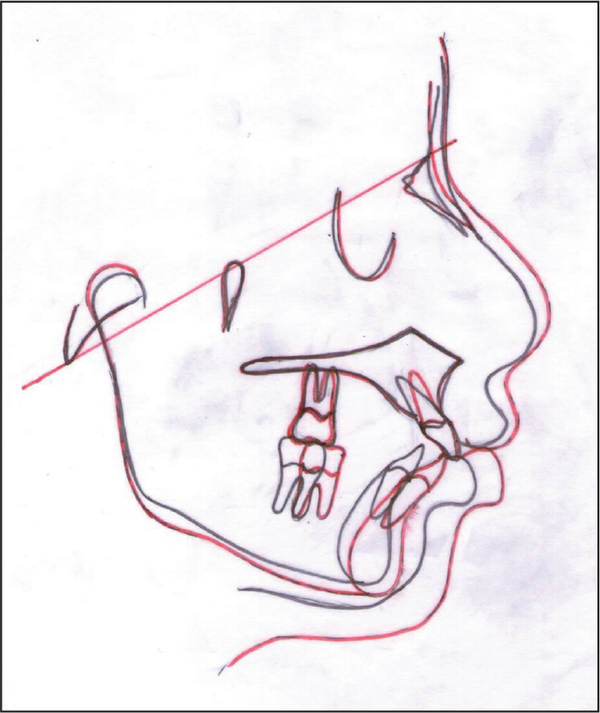
Overall Superimposition, Registered on the Sella-Nasion Line at Nasion
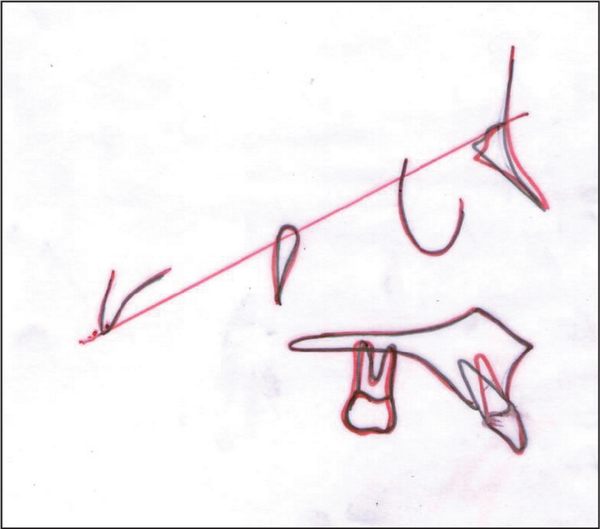
Cephalometric Superimposition: Maxillary Superimpositions. Registered on Ba-N at n Point
Cephalometric Superimposition: Maxillary Superimpositions. Registered on the Palatal Plane at ANS
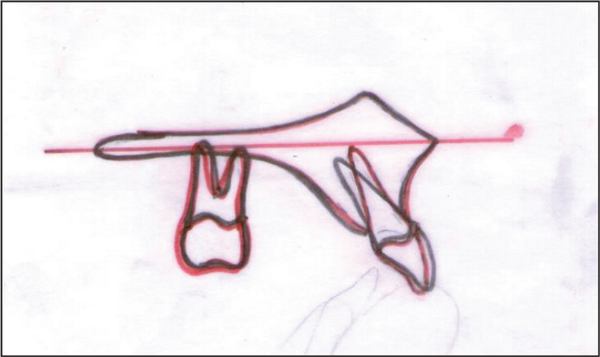
. Cephalometric Superimposition: Mandibular Superimpositions on the Corpus Axis at pm
Critical Appraisal
PK was successfully treated by both skeletal and dental corrections. The original treatment aim was accomplished and patient’s complain was addressed. PK was notably pleased with the treatment outcome. A good occlusal and aesthetic result was achieved and the same was reflected in the peer assessment reading and the index of orthodontic need scores. Andrews’ 6 keys to normal occlusion were satisfied in the posttreatment and postretention occlusion.
Skeletal: The sagittal skeletal pattern was corrected to skeletal Class I. Advancement of Point B due to downward and backward rotation of mandible explains the cephalometric sagittal correction.
Dental: The overjet of 8 mm was successfully reduced to the normal limit. The final anterior tooth fit was good. Posteriorly by finishing to the Class I molar relationship meant that the occlusal fit was good. Buccal segment interdigitation was reasonable and further settling was anticipated.
Soft tissue: Harmonious soft tissue esthetics were achieved at the end of the treatment. There was a significant improvement in the profile of the patient. The lips were competent with an ideal incisal exposure during posed smile.
Conclusion
Growth modification is a successful approach for treating young individuals with Class II skeletal malocclusion. Mandibular advancement can be successfully achieved by using various myofunctional appliances. In this case, the use of twin-block appliance in the functional phase helped to achieve harmonious skeletal, dental, and soft-tissue balance.
References
- 1. Staley R. Etiology and prevalence of malocclusion. In: Bishara S, ed. Textbook of Orthodontics. Philadelphia, PA: W.B. Saunders; 2001:83.
- 2. McNamara J. Component of Class II malocclusion in children 8-10 years of age. Angle Orthod. 1981;51(3):177–202.
- 3. Proffit WR. Treatment of skeletal problems in children. In Proffit WR, ed. Contemporary Orthodontics. 4th ed. St. Louis, MO: Elsevier; 2007:510–521.
- 4. Graber TM, Rakosi T, Petrovic AG. Dentofacial orthopedics with functional appliances. Principles of Functional Appliances. St. Louis, MO: Mosby; 1985.
- 5. O’Brien K, Wright J, Coboy F Early treatment for Class II Division 1 malocclusion with the Twin-block appliance: A multi-center, randomized, controlled trial. Am J Orthod Dentofacial Orthop. 2009;135(5):573–579.