In nursing education, fostering nursing students' competence of independently caring for patients is crucial (; ). To become quality nurses, nursing students need to develop several core competencies, professional knowledge, and skills to comprehensively identify and deal with the diseases and symptoms presented by clinical patients; such training content involves basic medical, surgical, and maternal care knowledge, as well as nursing skills (). When faced with complex clinical cases, due to the urgency of clinical situations and the lack of practical experience, nursing students may deal with the cases ineffectively or even incorrectly (). Students might enter the clinical setting and merely mimic the experiences of others, attempting to learn by imitation to identify the primary health issues associated with cases and determine which nursing measures are feasible. Therefore, it is important for nursing educators to teach students how to effectively apply their knowledge to solve case problems, which is a crucial task for nursing educators.
Critical reflection is a core aspect of nursing education (). However, owing to students' lack of cognition and experience, they often cannot engage in effective critical reflection (). Therefore, nursing educators have proposed various strategies to enhance students' critical reflections (; ). Among these strategies, engaging students in creating patient characters is commonly used in nursing education to promote critical thinking (). Patient character creation refers to the process of describing patients' personal information and characteristics, such as diagnostic results, age, occupation, history of smoking and alcohol consumption, family medical history, basic information, reasons for seeking medical care, medical history, and reasons for hospitalization (; ).
Due to the complexity of some medical conditions, which are not easily conveyed to students through oral instruction alone, third-party vendors have developed various programs incorporating personas in clinical scenarios to assist teachers in educating students. For example, Sunnqvist et al. () conducted a study using virtual patients with psychiatric characteristics to enhance students' collaborative learning and critical thinking. John and Mathew () engaged students in identifying patient characteristics through virtual patients to improve their critical thinking. Hosseini et al. () also used virtual patient characters in case analysis tasks to enhance students' clinical decision-making skills. With the development of holistic care concepts, using patient characters in nursing education has been considered an effective way to help nursing students face complex cases, consider and collect patient history data, and identify the true nursing health problems of specific cases ().
Research has established that conventionally created personas such as humanoid diagrams differ from traditional nursing education concept maps. They not only visually present case care needs, but also train students to comprehensively understand priority care issues from various perspectives (). This helps students relate a patient's medical history, nursing diagnoses, and needs. Virtual patients have been developed to represent a case's medical information using images, text, and language (; ). Nursing students integrate patient personas into their professional thinking activities to solve health problems (). Without the effective use of patient characters, students cannot successfully address the health issues of cases.
Encouraging students to use patient characters when solving health problems can help them organize crucial information about their cases (). Students who use patient characters and evidence-based professional knowledge tend to have better problem solving abilities; that is, patient characters can be considered as a visual knowledge representation tool (). The current nursing education literature mostly explores the effectiveness of using patient characters by creating personas through case report analysis. According to the literature, the lack of clinical experience and scenarios leads nursing students to experience difficulties in directly obtaining clinical knowledge (), self-efficacy (), problem solving abilities, and decision-making skills during class (). In addition, there is a lack of experimental design studies that analyze the effects on learning outcomes. Thus, the effects of patient character-based teaching strategies via persona creation on students' abilities to solve health problems remain unclear, particularly regarding obstetric care clinical reasoning.
In response to the advent of the artificial intelligence (AI) era, using generative AI patient-character tools to create personas can assist teachers in helping students construct and reorganize their knowledge (). Generative AI-based personas can facilitate the integration of complete case information and, through more structured information, help students understand the diversity of complex cases and develop empathy, thereby preparing them for clinical work (). Computers can aid in the construction of patient characters by creating personas. Computerized patient characters are widely recognized as a beneficial tool for learners to obtain more structurally complete case information and support clinical decision making. To date, there have been no domestic or international studies on the application of generative AI-assisted patient characteristics to assist in the creation of personas. Therefore, this study applied generative AI to patient character activities to develop nursing students' clinical knowledge, self-efficacy, problem solving abilities, and decision-making skills in patient management. The research questions were:
What are the differences in the clinical knowledge of nursing students using the generative artificial intelligence-based patient character creation (GAI-PCC) teaching strategy and those using the conventional creating personas teaching strategy (C-CPTS)?
What are the differences in the self-efficacy of nursing students using the GAI-PCC teaching strategy and those using the C-CPTS?
What are the differences in the problem solving abilities of nursing students using the GAI-PCC teaching strategy and those using the C-CPTS?
What are the differences in the decision-making skills of nursing students using the GAI-PCC teaching strategy and those using the C-CPTS?
Literature Review
Cooper () first introduced the concept of personas, describing personas as a tool for understanding and predicting user behavior to design products that better meet user needs. This concept was quickly adopted by the design community and integrated into the design thinking process. Scholars have proposed creating personas via patient characters to teach students how to integrate various types of knowledge and skills to make judgments and decisions, and to provide effective care (). Patient character creation involves the use of fictional or real patient profiles to simulate clinical scenarios (). In medical terminology, “patient character creation” refers to the careful observation and recording of case symptoms. This includes collecting information on the symptoms described by patients and observing specific features, qualities, or characteristics, such as the nature, location, duration, intensity, and progression of symptoms. These observations can help nursing students gather information to differentiate diseases, facilitate clinical practice and diagnosis, and aid in differential diagnosis and treatment ().
The use of patient characters in medical and nursing education can lead to more effective teaching outcomes. Mayer () reported that students learn better with graphics, which more effectively trigger brain memory, than with words alone, making the learning process meaningful and significant. Tang et al. () presented empirical case analyses of the human-oid diagram teaching strategy, demonstrating its effectiveness in terms of improving novice nurses' nursing care knowledge and technical skills. The patient character teaching strategy differs from the humanoid diagram teaching strategy because it focuses on a holistic view of the patient's medical history, symptoms, and personal context. Scholars have indicated that application of the patient character teaching strategy in nursing activities prepares students for real-life clinical situations and patient interactions ().
Patient-centered care in health sciences education that adopts strategies using patient characters combined with technological applications has received support from various studies (). For instance, the use of virtual patients in nursing education through simulated interactive learning scenarios was found to strengthen clinical training and improve students' relational skills (). Introducing students to patient characters early effectively integrates them into clinical practice, helping them adapt to complex patient care scenarios. For example, Foster et al. () used virtual patient characters to teach students empathy, and Chon et al. () used a web-based immersive patient simulator as a curricular tool to improve student performance in objective structured clinical examinations. Similarly, El-sol and Mohmmed () used critically ill patient characters to educate nurses on knowledge, attitudes, and practices regarding physical restraints. Chaby et al. () used embodied virtual patients as a simulation-based framework to enhance clinician-patient communication skills.
Standardized patients and therapeutic communication training have been validated for teaching specific patient care priorities to nursing students. This consistent training approach cultivates students' therapeutic communication skills through debriefing sessions (). Researchers have studied web-based standardized patient simulation with interactive roles to assess its efficacy in training skills, such as patient data collection and diagnosis ().
Thus, patient characters serve as a tool to help students interpret patients' illness narratives and understand their clinical needs. By collecting and compiling patient character stories, students are trained to engage in professional reflection, thereby creating nursing services that are professional, empathetic, and of high quality (; ). This preparation enables students to assess patient conditions quickly and accurately, and to identify problems when they enter the workforce. Memories retained through observation and performance form an organized whole, allowing students to judge and manage patients' overall situations, thereby enhancing their confidence and abilities in future health care practice. Therefore, this study aimed to explore how patient characters can help teachers develop students' practical and interpersonal skills in a clinical setting via the creating personas teaching strategy, which emphasizes clinical practice and patient care through interactive and scenario-based learning.
Method
The GAI-PCC Teaching Strategy via a Self-Directed Learning (SDL) Framework
The teaching strategy used in this study incorporated generative AI with Garrison's () SDL model, which includes three dimensions: (1) learning motivation; (2) self-management; and (3) self-monitoring (Figure 1). Learning objectives, along with the provision of immediate feedback and resource management, can enhance self-monitoring and allow students to engage in metacognitive reflection on their learning. Additionally, the patient character method based on generative AI is implemented using ChatGPT in an online environment, integrating SDL strategies into Xmind, which is a popular mind mapping and brainstorming software tool that helps users visually organize and structure their thoughts, ideas, and information (; ).
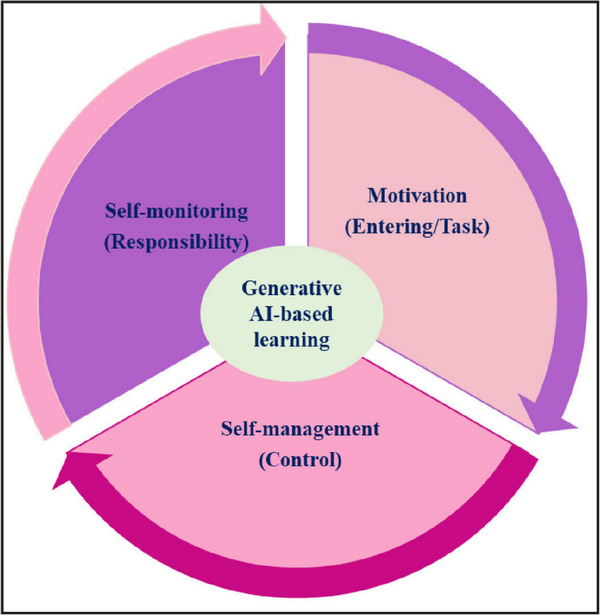
Figure 1
Generative artificial AI-based self-directed learning model intelligence.
Note. AI = artificial intelligence.
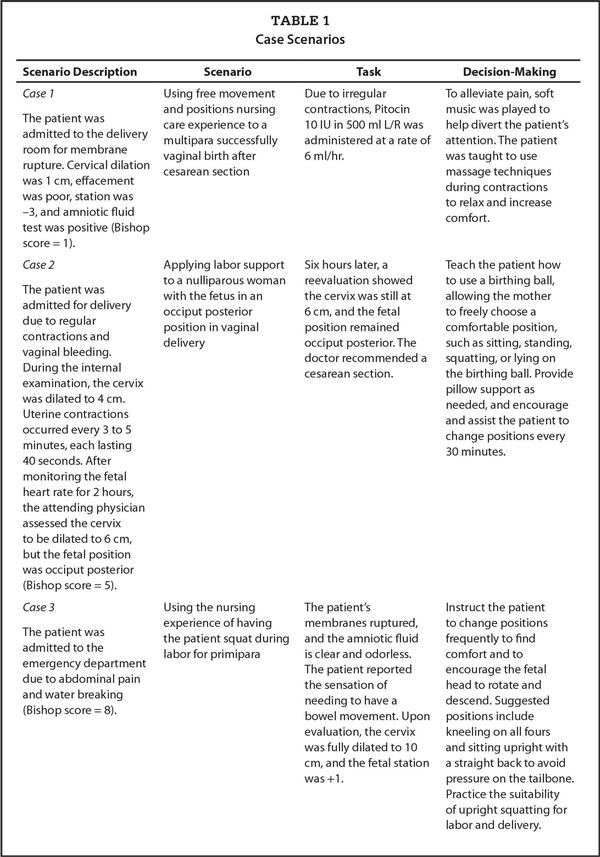
In the learning motivation phase, students engaged in this practice by setting learning goals and managing their learning resources. Real-life clinical cases stimulate students' learning motivation (Table 1). To simulate various real-life scenarios and the different severity levels that a woman in labor may face, character profiles were designed for case studies and education, allowing students to gain a comprehensive understanding of a maternal case. The Bishop score system was used to evaluate labor progress, including cervical effacement and dilation, and the descent of the fetal head (). Additionally, the patient character scenario design considered the most common fetal heart rate changes and their contraction progress during obstetric care, such as the management of fetal heart rate abnormalities. These abnormalities often occur during labor induction events, such as the use of Pitocin and pain management techniques ().
The character scenario included self-regulated (SRL) education strategies for decision-making skills. These strategies ensure that cases are communicated using brief, simple, and familiar language through direct face-to-face interactions and using structured questions to correctly and appropriately convey understandable content and provide straightforward guidance. As presented in Table 1, the simulation included three different character scenarios for women in labor, covering situations ranging from fetal heart rate abnormalities to severe interventions. Specific decision-making strategies were paired with the best treatment for each case. Images and digital health education tools also could be used to help understand fetal heart rate changes.
In the self-management phase, through characters' scenario creating personas drawing activities, students were self-managed to define the real problems in each case and to provide the best treatment and nursing care. In the last week, all of the students were invited to participate in the discussion of their roles and duties as well as the experience of playing a role in the case study activity for more interactive and active participation and critical thinking.
Students were instructed to download and learn to use computer-aided concept software including Xmind (https://xmind.app/download/) and were taught how to embed external images into diagrams created within the software and export these diagrams as PDFs, PNGs, or other image files. Students were guided in self-managing the correct use of Xmind (Figure 2).
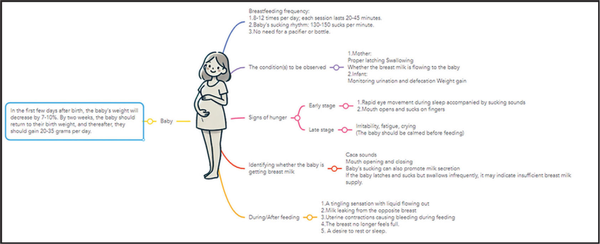
Figure 2
Screenshot of the student Xmind activity by case scenario.
In the self-monitoring phase, students integrated Generative AI, specifically through ChatGPT, with SDL to create personas. The aim was to equip students with critical thinking and problem solving abilities in obstetric clinical practice. The Generative AI guided students through the instructional activities and learning sheets to complete patient character drawings in an evidence-based labor care scenario for obstetric patients. As an assignment, students were required to create an obstetric character scenario. The students had to search a database for an evidence-based case report titled, “Using Free Movement and Positions Nursing Care Experience for a Multipara Successfully Vaginal Birth After Cesarean Section” and upload the case report to ChatGPT, request the creation of a mind map, copy it into a text file, save it as a mark-down format file, and import it into Xmind to obtain Figure A (available in the online version of this article).
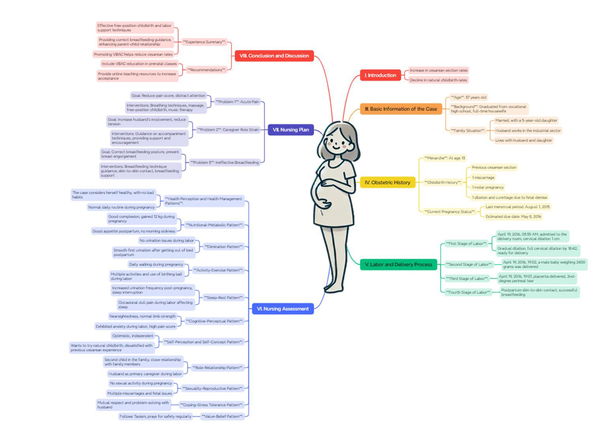
Figure A
A student-patient character scenario activity using GAI-PCC AI-based patient character creation.
Note. GAI-PCC = generative artificial intelligence-based patient character creation; AI = artificial intelligence.
Experimental Design
The 5-week experimental process is outlined in Figure 3. First, the obstetrics instructor introduced knowledge of obstetric case care. After assistance with group formation, students completed pretest questionnaires and assessments. Before the study began, students received a 2-hour lesson that included using computers to scaffold and depict obstetric character scenarios, as well as methods and basic concepts for creating them. This involved drawing hierarchical relationships in the obstetric character scenarios and linking similar concepts with lines and labels. During the class, students practiced drawing obstetric character scenarios, guided by the instructor.
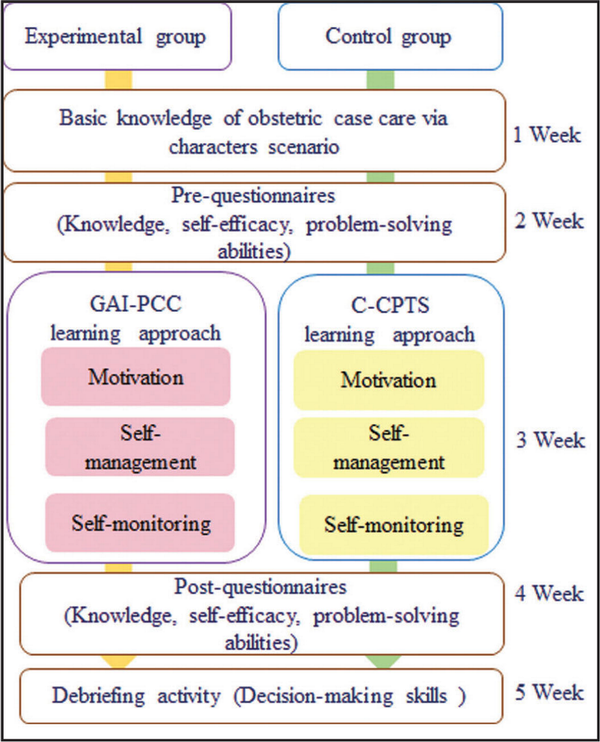
Figure 3
Procedure of the experiment design.
Note. GAI-PCC = generative artificial intelligence-based patient character creation. C-CPTS = conventional creating personas teaching strategy.
In the second week, students completed tasks based on the learning sheets and searched databases for evidence-based obstetric case studies. In the third week, the experimental group used the GAI-PCC learning approach to create character scenarios through ChatGPT and Xmind during the motivation, self-management, and self-monitoring phases. The control group used the C-CPTS learning approach to perform the same activity, but students only used Xmind to create character scenarios during these phases. In the fourth week, students completed their character scenarios and engaged in debriefing, reflection, and feedback activities to discuss the obstetric care skills learned from the activity. After the fifth week, both groups of students completed posttest questionnaires and surveys to assess their learning outcomes.
Participants
The sample sizes for the two groups were calculated to ensure an alpha level of 0.05 and statistical power of 80%, with each group targeting a medium effect size (Cohen's d = 0.5). A convenience sampling approach was used for this study. Initially, 70 third-year nursing students with an average age of 20 years enrolled in two classes at a nursing school in northern Taiwan were invited to participate. A single researcher contacted all of the students to obtain consent. Of the 70 students who were approached, two students chose not to participate, resulting in 68 students initially agreeing to join the study. After further exclusions due to personal reasons, such as issues with course credits or a lack of interest after receiving additional details about the study, 66 students participated in the study.
The participants were assigned from two classes, with 33 students from one class assigned to the experimental group using the GAI-PCC method, and 33 students from the second class assigned to the control group using the C-CPTS method. All of the students were willing to participate in the survey and were jointly enrolled in a three-credit obstetric nursing course. Obstetric nursing training is a compulsory course required for nursing certification and an important component of nursing education. To verify the effectiveness of the GAI-PCC method, a quasiexperimental design was proposed. A pretest/posttest study was conducted to examine differences in students' knowledge, self-efficacy, problem solving abilities, and decision-making skills.
Measuring Tools
Knowledge was evaluated using pre- and posttests designed by two experienced obstetric nursing instructors, each with more than 10 years of clinical experience. The content validity of the knowledge items was confirmed through the opinions of two maternal care experts, achieving an expert validity index (EVI) of 0.80, which indicates a high level of content validity in the design of the test. Moreover, the internal reliability of the knowledge items was calculated using the Kuder-Richardson Formula 20 (KR-20), with the estimated reliability of the items, based on test-retest, reported as 0.78 to 0.76. This knowledge test aimed to assess the students' basic knowledge of obstetric care. Each test comprised 10 multiple-choice questions; if the students answered all questions correctly, the total score was 100 points. The questions for the pre- and posttests were identical; however, the posttest questions were randomly arranged. For example, one of the knowledge test items was:
A pregnant woman is admitted for delivery due to regular contractions and vaginal bleeding. During internal examination, the cervix is dilated to 4 cm, with uterine contractions occurring every 3 to 5 minutes, each lasting 40 seconds. After monitoring the fetal heart rate for 2 hours, the attending physician reassesses the cervix, finding it dilated to 6 cm, but the fetal position is occiput posterior (Bishop score of 5). Based on this information, the most appropriate next step in the management of this patient is (A) perform a cesarean section due to the fetal position; (B) administer oxytocin to increase the frequency and intensity of contractions; (C) encourage the patient to walk to help facilitate the labor progress; or (D) provide pain management and continue monitoring the labor progress. The correct answer is D.
Students' self-efficacy and problem solving abilities in obstetric care also were measured using a 5-point Likert scale ranging from 1 = strongly disagree to 5 = strongly agree. Self-efficacy was assessed using eight items proposed by Pintrich et al. (). Sample items included, “I am confident I can understand the most complex material presented by the instructor in this course,” and “I am confident I can do an excellent job on the assignments and tests in this course.” Cronbach's alpha for these questionnaires was .90, indicating high reliability. The scale has shown strong reliability and validity, with its effectiveness confirmed in various international studies across diverse participant groups (; )
The problem solving questionnaire, designed by Lai and Hwang (), included five items, such as “I will not escape from the problems I encounter” and “I always try my best to solve the problems I encounter.” Cronbach's alpha for this questionnaire was .91, indicating high reliability. This scale exhibits strong reliability and validity as evidenced by its validation in multiple international studies involving various participant groups (; ).
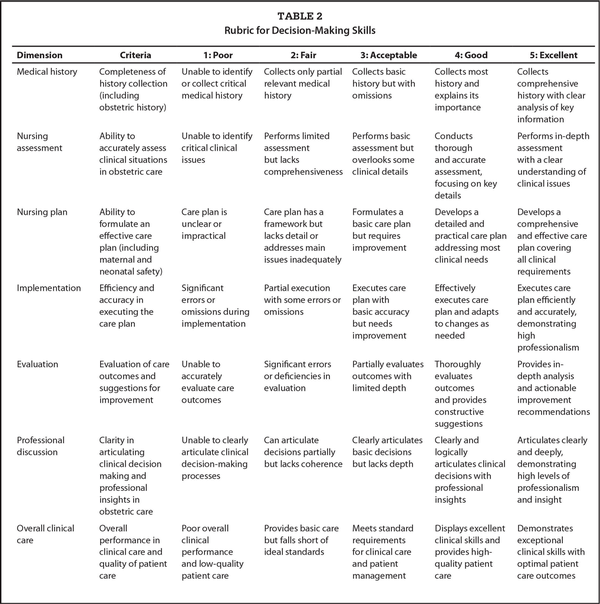
Decision-making skills were assessed during a debriefing activity using the case-based discussion tool to evaluate clinical judgment ability. This measure was modified from Tang et al. () and is based on insights from two specialists who used it as a reliable and effective tool to train newcomers. The kappa coefficient was 0.93, indicating consistent reliability among the experts. In addition, the rubrics were validated by two experts in maternal care education, obtaining an expected value of information (EVI) of 0.82, which reflects a strong consensus among the experts regarding content validity. The scores ranged from 1 to 5, with higher scores indicating better reflective decision-making skills based on students' debriefing activity. The study measured students' decision making and application of obstetric-care knowledge in clinical situations using seven items: (1) medical history; (2) nursing assessment; (3) nursing plan; (4) implementation; (5) evaluation; (6) professional discussion; and (7) overall clinical care (Table 2).
Ethical Considerations
The study was approved by Taipei Medical University's Ethics Committee. Students voluntarily chose to participate, and informed consent was obtained from all of the participants, who could withdraw from the study at any time without limitations. The study adhered rigorously to the ethical principles specified in the Declaration of Helsinki and its subsequent amendments.
Data Analysis
Data analysis was conducted using SPSS® version 21 for both descriptive and inferential statistical techniques. The independent-samples t test was used to compare the two groups' scores for knowledge, self-efficacy, problem solving abilities, and decision-making skills. A p < .05 was regarded as statistically significant, suggesting that the observed differences were unlikely to be due to random variation, thus enhancing the credibility of the findings.
Results
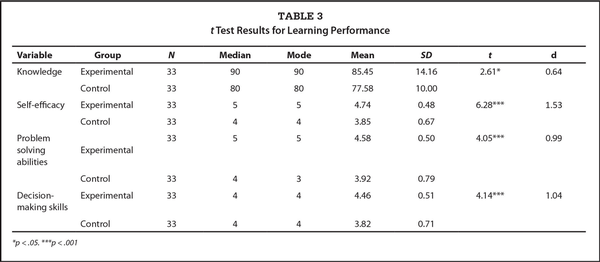
Independent-samples t tests for the pretest scores of knowledge, self-efficacy, problem solving abilities, and decision-making skills showed no statistically significant differences between the two groups (t = 1.37–3.28, p > .05). Thus, the two groups' initial knowledge, self-efficacy, problem solving abilities and decision skills were considered to be equivalent.
An independent-samples t test was conducted on the post-test scores of the two groups. As demonstrated in Table 3, the t test result revealed a significant difference (t = 2.61, p < .05) between the experimental group (M = 85.45 [SD = 14.16]) and the control group (M = 77.58 [SD = 10]). Similarly, the self-efficacy scores for the experimental group (M = 4.74 [SD = 0.48]) and the control group (M = 3.85 [SD = 0.67]) were significantly different (t = 6.28, p < .01). The problem solving abilities for the experimental group (M = 4.58 [SD = 0.50]) and the control group (M = 3.92 [SD = 0.79]) were significantly different (t = 4.05, p < .01). The decision-making skills for the experimental group (M = 4.46 [SD = 0.51]) and the control group (M = 3.82 [SD = 0.71]) also were significantly different (t = 4.14, p < .01). Therefore, the GAI-PCC method significantly improved nursing students' knowledge, self-efficacy, problem solving abilities, and decision-making skills.
Discussion
This study proposed the generative AI-based teaching strategy by integrating ChatGPT with SRL and evaluated its effectiveness using a quasiexperimental method involving university nursing students in obstetric care. The results demonstrated that compared with the C-CPTS learning approach, the GAI-PCC learning approach significantly enhanced nursing students' knowledge, self-efficacy, problem solving abilities, and decision-making skills. The integration of GAIPCC learning strategies and immersive scenarios provided students with the knowledge needed for academic success in nursing education and essential soft skills for building nursing students' competency.
Using the characters scenario learning method with the GAI-PCC approach has multiple educational benefits. For example, the character scenarios can be created and organized effectively for helping students manage and organize information systematically and visually to promote meaningful learning (). Graphical character scenarios with personas serve as graphical representations of learner understanding, enabling students to describe their understanding of concepts, and promoting knowledge construction. Additionally, graphical character scenarios can provide an in-depth understanding of students' learning performances and help educators improve their teaching to assist students in better understanding difficult knowledge and deeper learning expertise (). Overall, using the GAI-PCC approach, the character scenarios not only could enhance students' conceptual understanding and promote the integration of prior knowledge, knowledge reconstruction, and self-regulation, but also could potentially improve students' overall learning performance ().
Additionally, GAI-created character scenarios could ameliorate the time-consuming task of preparing materials. In response to the current era of generative AI, this article proposes a teaching method that is different from the conventional patient characters of the past by incorporating the GAI-PCC teaching strategy in an obstetric course. The results indicate this approach has great potential for improving students' knowledge, self-efficacy, problem solving abilities, and decision-making skills. In this study, students who used the GAI-PCC teaching strategy had significantly higher scores in knowledge, self-efficacy, problem solving abilities, and decision-making skills than students who used the traditional patient character teaching strategy. Therefore, GAI-PCC combined with generative AI significantly improved nursing students' knowledge, self-efficacy, problem solving abilities, and decision-making skills. Consistent with the findings of Liang et al. () and Topaz et al. (), the use of generative AI in nursing education can help in explaining complex topics, creating personal experiences, and improving communication skills. AI and generative language models provide opportunities for realistic simulations, personalized feedback, and immersive learning environments in medical education. Therefore, there was an overall improvement in the students' learning outcomes.
The results showed the GAI-PCC method is an effective teaching strategy that can improve nursing students' abilities in all respects to better cope with challenges in actual clinical situations. Based on these findings, the widespread application of generative AI technology combined with teaching strategies in nursing education can promote students' comprehensive development and improve their clinical abilities.
Additionally, future research can further explore the application effects of different types of GAI-PCC teaching strategies and the potential of these technologies for teaching other medical fields. Through continuous exploration and innovation, progress and changes can be made in medical education, and the quality of overall medical services can be improved.
Limitations
Although this study demonstrated the effectiveness of the GAI-PCC teaching strategy in improving nursing students' knowledge, self-efficacy, problem solving abilities, and decision-making skills, there are still some limitations that need to be considered. First, the sample size was relatively small and was limited to specific nursing students. Therefore, the generalizability of these results may be limited. In the future, samples with larger scales and from different regions will be needed to verify the stability of the research results. Second, because this study used an independent-samples t test, the research results might have been affected by factors such as the students' personal background, learning motivations, and previous learning experience. Therefore, future research should consider using randomized controlled trials to control for potential variables. Third, the data collection method used in this study relied primarily on questionnaires. Future research should consider combining other qualitative interview methods to obtain more comprehensive and reliable data. Although the results of this study demonstrate the potential advantages of GAI-PCC, the above limitations still need to be overcome, and more in-depth and extensive research must be conducted to comprehensively verify and enhance the application value of generative AI technology in nursing education.
Conclusion
Training students to obtain nursing licenses and enter the workplace is difficult. The results of this study show that the GAI-PCC teaching strategy effectively improves students' knowledge, self-efficacy, problem solving abilities, and decision-making skills. The use of the GAI-PCC teaching strategy allows students to have an integrated view of the nursing experience and the overall learning of clinical cases, thereby improving their clinical competency assessment and judgment skills. The GAI-PCC teaching strategy can be used in nursing courses to increase connections and integrate students' past internship experience and knowledge, strengthen their memory of the learning process, and achieve training effects.
This study lends initial support to the GAI-PCC teaching strategy as being effective and being able to comprehensively improve nursing students' knowledge, self-efficacy, problem solving abilities, and decision-making skills. The findings provide strong support for the widespread application of generative AI technology in nursing education. Future research should continue to explore the application effects of the GAI-PCC teaching strategy in different educational environments and student groups. For example, the GAI-PCC teaching strategy can be used as a regular teaching method for novice nurses. This teaching strategy should be further optimized to promote the development and progress of nursing education.
Overall, this study highlights the potential effects of generative AI technology on nursing education and provides new ideas and methods for improving nursing students' clinical abilities and professionalism. Through continuous exploration and innovation, further investigation into educational research applications based on generative AI technology will contribute to the development of highly qualified nursing professionals.
References
- Ahmady , S., Shahbazi , S. (2020). Impact of social problem-solving training on critical thinking and decision making of nursing students. BMC Nursing, 19(1), 94. 10.1186/s12912-020-00487-x PMID:
- Al-Bedaery , R., Baig , S., Khare , Y., Sullivan-Mchale , J. (2024). Humanising case-based learning. Medical Teacher, 46(10), 1348–1355– Advance online publication. 10.1080/0142159X.2024.2308066 PMID:
- Bartels , S. L., Taygar , A. S., Johnsson , S. I., Petersson , S., Flink , I., Boersma , K., McCracken , L. M., Wicksell , R. K. (2023). Using personas in the development of eHealth interventions for chronic pain: A scoping review and narrative synthesis. Internet Interventions: The Application of Information Technology in Mental and Behavioural Health, 3 2, 100619. 10.1016/j.invent.2023.100619 PMID:
- Berdida , D. J. E., Grande , R. A. N. (2023). Nursing students' nomophobia, social media use, attention, motivation, and academic performance: A structural equation modeling approach. Nurse Education in Practice, 70, 103645. 10.1016/j.nepr.2023.103645 PMID:
- Brennan , B. A. (2022). The impact of self-efficacy based prebriefing on nursing student clinical competency and self-efficacy in simulation: An experimental study. Nurse Education Today, 109, 105260. 10.1016/j.nedt.2021.105260 PMID:
- Brown , W. J., Tortorella , R. A. (2020). Hybrid medical simulation–A systematic literature review. Smart Learning Environments, 7, 16. 10.1186/s40561-020-00127-6
- Chaby , L., Benamara , A., Pino , M., Prigent , E., Ravenet , B., Martin , J. C., Vanderstichel , H., Becerril-Ortega , R., Rigaud , A.-S., Chetouani , M. (2022). Embodied virtual patients as a simulation-based framework for training clinician-patient communication skills: An overview of their use in psychiatric and geriatric care. Frontiers in Virtual Reality, 3, 827312. 10.3389/frvir.2022.827312
- Chan , M. M. K., Wong , I. S. F., Yau , S. Y., Lam , V. S. F. (2023). Critical reflection on using ChatGPT in student learning: Benefits or potential risks? Nurse Educator, 48(6), E200–E201–. 10.1097/NNE.0000000000001476 PMID:
- Chang , C. Y., Jen , H. J., Yang , J. C. (2024). Integrating scenario game-based learning with the experiential learning strategy to facilitate nursing students' learning performance and core competencies in labor support training. Interactive Learning Environments, 32(10), 7170–7185–. 10.1080/10494820.2024.2308092
- Chang , C. Y., Setiani , I., Darmawansah , D., Yang , J. C. (2024). Effects of game-based learning integrated with the self-regulated learning strategy on nursing students' entrustable professional activities: A quasi-experimental study. Nurse Education Today, 139, 106213. 10.1016/j.nedt.2024.106213 PMID:
- Chon , S. H., Hilgers , S., Timmermann , F., Dratsch , T., Plum , P. S., Berlth , F., Datta , R., Alakus , H., Schlößer , H. A., Schramm , C., Pinto Dos Santos , D., Bruns , C., Kleinert , R. (2018). Web-based immersive patient simulator as a curricular tool for objective structured clinical examination preparation in surgery: Development and evaluation. JMIR Serious Games, 6(3), e10693. 10.2196/10693 PMID:
- Cooper , A. (1999). The inmates are running the asylum. Macmillan. 10.1007/978-3-322-99786-9_1
- Demiray , A., Ilaslan , N., Kızıltepe , S. K., Acıl , A. (2023). Web-based standardized patient simulation for taking anamnesis: An approach in nursing education during the pandemic. BMC Nursing, 22(1), 325. 10.1186/s12912-023-01486-4 PMID:
- Elbilgahy , A. A., Eltaib , F. A., Lawend , J. A. (2020). Challenges facing clinical nurse educators and nursing students in Egyptian and Saudi clinical learning environment: A comparative study. International Journal of Africa Nursing Sciences, 13, 100240. 10.1016/j.ijans.2020.100240
- El-sol , A. E. S. H., Mohmmed , R. G. A. (2018). Assessment of nurse's knowledge, attitudes, and practice regarding physical restraints among critical ill patients. Assessment, 4(1), 15–22–.
- Foster , A., Chaudhary , N., Kim , T., Waller , J. L., Wong , J., Borish , M., Cordar , A., Lok , B., Buckley , P. F. (2016). Using virtual patients to teach empathy: A randomized controlled study to enhance medical students' empathic communication. Simulation in Healthcare, 11(3), 181–189–. 10.1097/SIH.0000000000000142 PMID:
- Gaba , A., Costa , S. A., Schnoll , R., Dorfman , M. E., Cordova , S., Jakuboski , S., Spiegel , B., Joshi , A. (2023). Development and evaluation of an online simulated hospital unit for nutrition assessment training. Topics in Clinical Nutrition, 38(2), 133–143–. 10.1097/TIN.0000000000000315
- Gassas , R. (2021). Sources of the knowledge-practice gap in nursing: Lessons from an integrative review. Nurse Education Today, 106, 105095. 10.1016/j.nedt.2021.105095 PMID:
- Garrison , D. R. (1997). Self-directed learning: Toward a comprehensive model. Adult education quarterly, 48(1), 18–33–. 10.1177/074171369704800103
- Hamilton , A. (2024). Artificial intelligence and healthcare simulation: The shifting landscape of medical education. Cureus, 16(5), e59747. Advance online publication. 10.7759/cureus.59747 PMID:
- Hemond , J. A., Franchek-Roa , K. M., Caplin , D. A., Hobson , W. L. (2021). Teen actors teaching communication skills. Cureus, 13(11), e19515. 10.7759/cureus.19515 PMID:
- Hosseini , T. M., Ahmady , S., Edelbring , S. (2022). Teaching clinical decision-making skills to undergraduate nursing students via web-based virtual patients during the COVID-19 pandemic: A new approach to the CyberPatientTM simulator. Journal of Contemporary Medical Sciences, 8(1), 31–37–. https://jocms.org/index.php/jcms/article/view/1158
- Hsia , L.-H., Lin , Y.-N., Hwang , G.-J. (2021). A creative problem solving-based flipped learning strategy for promoting students' performing creativity, skills and tendencies of creative thinking and collaboration. British Journal of Educational Technology, 52(4), 1771–1787–. 10.1111/bjet.13073
- Irwin , P., Coutts , R. (2020). Learning alone together: A qualitative investigation exploring virtual connectedness. International Journal on Innovations in Online Education, 4(4). 10.1615/IntJInnovOnlineEdu.2021036472
- Ismail , I. I., Salama , S. (2023). Depiction of nervous system disorders in television medical drama: A content analysis of 18 seasons of Grey's Anatomy. Clinical Neurology and Neurosurgery, 224, 107569. 10.1016/j.clineuro.2022.107569 PMID:
- Jennings , M., Deeny , P., Tizzard-Kleister , K. (2020). Acts of care: Applied drama, ‘sympathetic presence’ and person-centred nursing. In Fisher A. Stuart, Thompson J. (Eds.), Performing care: New perspectives on socially engaged performance (pp. 187–203–). Manchester University Press.
- John , R. A., Mathew , B. R. (2021). The virtual patient–An innovative online learning approach. International Journal of Nursing Education and Research, 9(2), 230–233–. 10.5958/2454-2660.2021.00055.7
- Khanijahani , A., Iezadi , S., Dudley , S., Goettler , M., Kroetsch , P., Wise , J. (2022). Organizational, professional, and patient characteristics associated with artificial intelligence adoption in healthcare: A systematic review. Health Policy and Technology, 11(1), 100602. 10.1016/j.hlpt.2022.100602
- Klaeson , K., Berglund , M., Gustavsson , S. (2017). The character of nursing students' critical reflection at the end of their education. Journal of Nursing Education and Practice, 7(5), 55–61–. 10.5430/jnep.v7n5p55
- Kuba , K., Kirby , M. A., Hughes , F., Yellon , S. M. (2023). Reassessing the Bishop score in clinical practice for induction of labor leading to vaginal delivery and for evaluation of cervix ripening. Placenta and Reproductive Medicine, 2, 8. 10.54844/prm.2023.0353 PMID:
- Lai , C. L., Hwang , G. J. (2014). Effects of mobile learning time on students' conception of collaboration, communication, complex problem-solving, meta-cognitive awareness and creativity. International Journal of Mobile Learning and Organisation, 8(3), 276–291–. 10.1504/IJMLO.2014.067029
- Li , L., Song , Z., Liang , Y., Zhao , L., Qin , Y., Li , Q., Liao , X., Luo , Q. (2022). Application of the teaching mode combining “virtual simulation + emergency care simulator” in surgical nursing. Creative Education, 13(12), 3904–3914–. 10.4236/ce.2022.1312250
- Liang , J., Wang , L., Luo , J., Yan , Y., Fan , C. (2023). The relationship between student interaction with generative artificial intelligence and learning achievement: Serial mediating roles of self-efficacy and cognitive engagement. Frontiers in Psychology, 14, 1285392. 10.3389/fpsyg.2023.1285392 PMID:
- Lim , S. C., Mustapha , F. I., Aagaard-Hansen , J., Calopietro , M., Aris , T., Bjerre-Christensen , U. (2020). Impact of continuing medical education for primary healthcare providers in Malaysia on diabetes knowledge, attitudes, skills and clinical practices. Medical Education Online, 25(1), 1710330. 10.1080/10872981.2019.1710330 PMID:
- Liu , X., Zhang , Y., Wang , D., Liu , H. (2023). Effect of “Four Passes” training and assessment of nurse specialty knowledge on the cultivation of core competence of clinical nurses. Yangtze Medicine, 7(1), 43–53–. 10.4236/ym.2023.71005
- Lopez , M., Goh , P. S. (2024). Catering for the needs of diverse patient populations: Using ChatGPT to design case-based learning scenarios. Medical Science Educator, 34(2), 319–325–. 10.1007/s40670-024-01975-4 PMID:
- Ma , J., Lee , Y., Kang , J. (2023). Standardized patient simulation for more effective undergraduate nursing education: A systematic review and meta-analysis. Clinical Simulation in Nursing, 74, 19–37–. 10.1016/j.ecns.2022.10.002
- Macartney , M. J., Cooper , J. F., Namasivayam , P. (2021). Student nurse perceptions of video simulation and critical reflection for developing clinical-reasoning skills: A cross cohort study. Student Success, 12(1), 47–55–. 10.5204/ssj.1653
- Mayer , R. E. (2021). Evidence-based principles for how to design effective instructional videos. Journal of Applied Research in Memory and Cognition, 10(2), 229–240–. 10.1016/j.jarmac.2021.03.007
- Özkan , Ç. G., Kurt , Y., Bayram , A. (2022). Investigation of nursing students' perceptions of nursing by drawing method: Time journey with drawings. International e-Journal of Educational Studies, 6(11), 34–44–. 10.31458/iejes.1009954
- Panayi , A. C., Endo , Y., Huidobro , A. F., Haug , V., Panayi , A. M., Orgill , D. P. (2021). Lights, camera, scalpel: A lookback at 100 years of plastic surgery on the silver screen. European Journal of Plastic Surgery, 44(5), 551–561–. 10.1007/s00238-021-01834-0 PMID:
- Pintrich , P. R., Smith , D. A. F., Garcia , T., McKeachie , W. J. (1991). A manual for the use of the Motivated Strategies for Learning Questionnaire (MSLQ). National Center for Research to Improve Postsecondary Teaching and Learning.
- Rouleau , G., Gagnon , M. P., Côté , J., Richard , L., Chicoine , G., Pelletier , J. (2022). Virtual patient simulation to improve nurses' relational skills in a continuing education context: A convergent mixed methods study. BMC Nursing, 21(1), 1. 10.1186/s12912-021-00740-x PMID:
- Said , S. E. (2021). How to apply community-oriented medical education (COME). Journal of Clinical Case Reports and Clinical Study, 4(1), 1–4–. 10.61148/2766-8614/JCCRCS/062
- Shin , S., Lee , I., Kim , J., Oh , E., Hong , E. (2023). Effectiveness of a critical reflection competency program for clinical nurse educators: A pilot study. BMC Nursing, 22(1), 69. 10.1186/s12912-023-01236-6 PMID:
- Su , Z., McDonnell , D., Ahmad , J., Cheshmehzangi , A. (2023). Disaster preparedness in healthcare professionals amid COVID-19 and beyond: A systematic review of randomized controlled trials. Nurse Education in Practice, 69, 103583. 10.1016/j.nepr.2023.103583 PMID:
- Sunnqvist , C., Karlsson , K., Lindell , L., Fors , U. (2016). Virtual patient simulation in psychiatric care–A pilot study of digital support for collaborate learning. Nurse Education in Practice, 17, 30–35–. 10.1016/j.nepr.2016.02.004 PMID:
- Tang , Y. H., Chen , H. L., Chen , H. Y., Chuang , S. W., Liao , L. N., Huang , L. C. (2022). The effectiveness of humanoid diagram teaching strategy on care capacity and retention in novice nurses. Nurse Education in Practice, 58, 103272. 10.1016/j.nepr.2021.103272 PMID:
- Topaz , M., Peltonen , L. M., Michalowski , M., Stiglic , G., Ronquillo , C., Pruinelli , L., Song , J., O'Connor , S., Miyagawa , S., Fukahori , H. (2024). The ChatGPT effect: Nursing education and generative artificial intelligence. Journal of Nursing Education, 1–4–. Advance online publication. 10.3928/01484834-20240126-01 PMID:
- Wang , L., Wang , Y., Wang , X., Xue , C. (2023). Effects of mind mapping based on standardized patient program in patient education among postgraduate nursing students in clinical setting. BMC Medical Education, 23(1), 982. 10.1186/s12909-023-04944-4 PMID:
- Wang , X. M., Hu , Q N., Hwang , G. J., Yu , X. H. (2023). Learning with digital technology-facilitated empathy: An augmented reality approach to enhancing students' flow experience, motivation, and achievement in a biology program. Interactive Learning Environments, 31(10), 6988–7004–. 10.1080/10494820.2022.2057549
- Yang , K. H., Chen , H., Liu , C. J., Zhang , F. F., Jiang , X. L. (2022). Effects of reflective learning based on visual mind mapping in the fundamentals of nursing course: A quasi-experimental study. Nurse Education Today, 119, 105566. 10.1016/j.nedt.2022.105566 PMID:
- Yang , S. W., Kim , S. Y., Hwang , H. S., Kim , H. S., Sohn , I. S., Kwon , H. S. (2021). The uterocervical angle combined with Bishop score as a predictor for successful induction of labor in term vaginal delivery. Journal of Clinical Medicine, 10(9), 2033. 10.3390/jcm10092033 PMID: