Introduction
The sexual act is a psychobiological response. It is much more than the mechanical process of peno-vaginal intercourse and involves the formation of a special bond between the two partners. The sexual process is influenced by the biological and psychological framework of both the partners along with societal influences. Besides these environmental factors, emotional bonding, the perceived image of the self and partner and sexual preferences also play a pivotal role in experiencing the quality of the sexual act. A problem or mismatch in any of the aforementioned variable scan leads to sexual dysfunction.
Available data suggest a wide range for the prevalence of sexual dysfunction, which is influenced by ascertainment methods, age of the participants, presence or absence of various physical and psychiatric comorbidities. In general, it is suggested that about 43% of women and 31% of men have one or other kinds of sexual dysfunction, with premature ejaculation (PME) being the most common sexual dysfunction occurring in males and hypoactive sexual desire disorder (HSDD) in females. There is a disparity in data regarding the rates of different female sexual disorders in different studies.
Rating scales form an integral part of the assessment of various sexual dysfunctions. However, these should be used as an alternative to more thorough history taking and clinical examination. In routine clinical settings, the standardized rating scales can aid in the detection of symptoms, in serial monitoring, and evaluating the effectiveness of various treatment strategies (improvement or deterioration). Further, this rating may also provide objective evidence, which may be useful in medicolegal cases. In research settings, the use of standardized rating scales can help in comparison to the results of similar studies and can help in evaluating the efficacy of various treatment interventions.
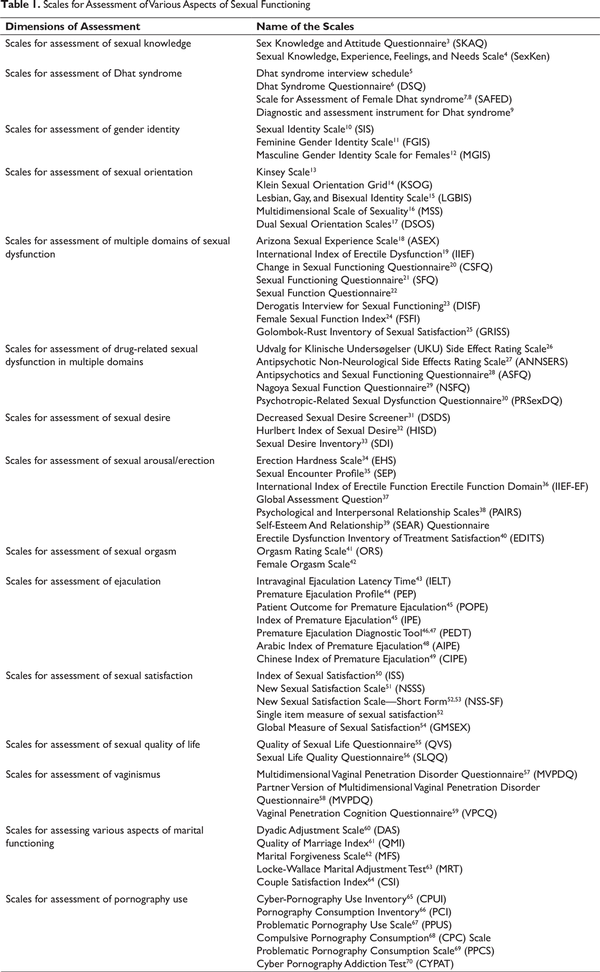
Over the years, various rating scales have been designed to assess different aspects of sexual dysfunction and other sexual disorders (Table 1). Some of these scales assess a specific aspect of sexual functioning, specific sexual dysfunction, or other aspects of sexual disorders, whereas others are more general, which assess multiple domains of sexual functioning (Table 1). It is also known that sexual functioning is often influenced by marital functioning or quality of relationship with the partner. In recent times, with the increase in the use of technology, pornography is also been shown to influence the various aspects of sexual relationships. Clinicians providing care to patients presenting with different aspects of problems in a sexual relationship are expected to evaluate all these aspects, before formulating a treatment plan. Due to the availability of multiple scales to assess the sexual problems, clinicians and researchers are often on the cross-roads while selecting a scale for use. This review attempts to review the available instruments for the assessment of various aspects of sexual functioning and compare their advantages and disadvantages. For this review, a PubMed and PsycINFO search was carried out using the keywords, sexual, dysfunction, screening, assessment, prevalence, incidence, risk factors, instruments, etiology, erectile dysfunction, PME, vaginismus, Dhat, Dhat syndrome, sexual knowledge, orientation, satisfaction, quality of life, pornography, marital, etc, in various combinations. Based on the available information the available data were organized. For better understanding, we organized the available scales as scales assessing multiple aspects of sexual dysfunction or those assessing specific aspect of sexual functioning, ie, sexual knowledge, scales evaluating Dhat syndrome, sexual orientation, sexual desire, sexual arousal/erection, sexual orgasm, ejaculation, sexual satisfaction, sexual quality of life, drug-related sexual dysfunction, and vaginismus. Scales evaluating marital relationships and viewing pornography are presented separately.
Scales for Sexual Knowledge
Sexual knowledge of a person influences his/her participation in a sexual act. People with poor sexual knowledge may present with any kind of sexual dysfunction or disorder, even when in reality, there is none. They can also contribute to the distress in the partner, either by avoiding sexual acts or by indulging in a more frequent sexual activity, than acceptable by the partner. Sexual knowledge refers to the information/knowledge about the related facts, clarity about the myths and misconceptions related to the sexual act and other aspects of sexuality. It is important to assess for sexual knowledge as it may be the reason for the onset of sexual and related pathology. Different scales have been developed to assess sexual knowledge. It is important to understand that sociocultural factors influence sexual knowledge. Hence, it is important to use scales, which are culturally valid and takes into account the locally prevalent myths and misconceptions. The commonly used scales for assessment of sexual knowledge are Sex Knowledge and Attitude Questionnaire (SKAQ) and Sexual Knowledge, Experience, Feelings, and Needs Scale (SexKen).
Sex Knowledge and Attitude Questionnaire (SKAQ): This is a self-rated questionnaire, developed in India. It comprises of 2 subparts: knowledge subscale and attitude subscale. The knowledge subscale has 35 items with a dichotomous scoring system, with a maximum score of 35 points. The attitude subscale has a total of 20 items and is scored on a 3-point Likert scale (scoring: 1-3), with a maximum total score of 60 points. Higher scores are indicative of better sexual knowledge and a more liberal attitude. The scale is available in the Hindi language. It has test-retest reliability for the knowledge subscale is 0.433 and that for attitude as 0.665.
Sexual Knowledge, Experience, Feelings, and Needs Scale (SexKen): First it was designed to assess the sexual knowledge, experience, feelings, and needs of people with mild intellectual disabilities (SexKen-ID) and was later modified for use in general population (SexKen-GP) and also in people with physical disabilities (SexKen-PD). It assesses a variety of areas related to sexual functioning. It has 13 subscales and each of which comprises questions on experience, knowledge, feelings, and needs of respondents’ related to their area of sexuality. It takes around 1 hour to complete. It has good test-retest reliability and internal consistency.
Questionnaires for Assessment of Dhat Syndrome
“Dhat syndrome” is a culture-bound syndrome, characterized by the combination of somatic, anxiety, depressive, and sexual symptoms, all attributed to the loss of semen. This has been mainly reported by patients from the Indian subcontinent but is not limited to Indian only and has been reported in different other cultures too. It is also kept under the heading of “Glossary of Cultural Concepts of Distress” in DSM5. Though not common in the West, it can be associated with significant distress. Many instruments have been developed to assess the various components of Dhat syndrome.
Dhat Syndrome Interview Schedule: This was developed as a 13-item semistructured interview schedule for assessment of Dhat syndrome (DSIS), which has high inter-rater reliability.
Dhat Syndrome Questionnaire (DSQ): It is a self-rated questionnaire designed for a comprehensive assessment of Dhat syndrome. It assesses the personal beliefs about the characteristics of Dhat, situations in which the person experiences passage of Dhat, logic behind the passage of Dhat, accompanying symptoms, sequelae of the passage of Dhat, and treatment-related and help-seeking beliefs. The average time for completion is 10 minutes. It is available in 10 Indian languages and has good content validity.
Scale for Assessment of Female Dhat syndrome (SAFED), : This is a modified version of DSQ. It is used for assessment of beliefs, associated symptoms, and other features in patients with nonpathological vaginal discharge. It has similar properties as that of DSQ.
Diagnostic and Assessment Instrument for Dhat Syndrome: This instrument was developed to assess the phenomenology of Dhat syndrome. It has 2 subscales, ie, health beliefs scale and associated symptoms scale. Both the subscales have a 3-factor structure. Based on the severity of symptoms, patients can be categorized into 3 clusters.
Scales for Sexual Identity
Gender identity means the patient’s perception of his psychosexual identity as being a male or a female. It can be a reason for sexual dysfunction in a heterosexual couple as a physiological male who has a gender identity of a female may not be able to perform in the sexual intercourse with a physiological female who has a sexual identity of a female. This area is generally overlooked in the assessment and management of patients presenting sexual problems and should not be neglected. Available instruments for assessing gender identity include Sexual Identity Scale (SIS), Feminine Gender Identity Scale (FGIS), and Masculine Gender Identity Scale for Females (MGIS).
Sexual Identity Scale (SIS): This scale was developed in 1987 and comprises of 4 functional sex dimensions. Reliability, assessed with Cronbach’s α, is high. Construct validity, both convergent and divergent validity, is good.
Feminine Gender Identity Scale (FGIS): This scale assesses the extent of feminine traits in males. It has 29 questions, divided into 3 subparts, A, B, and C. It takes about 15 minutes for completion. Higher scores in a particular domain indicate that the particular attribute (eg, sadism, feminine gender identity) is present to a greater extent, and low scores indicate otherwise.
Masculine Gender Identity Scale for Females (MGIS): This scale was developed to measure “masculinity” in homosexual females. MGIS was developed as a partner instrument to the FGIS. The MGIS is a self-administered, multiple-choice questionnaire measure. It comprises of 2 subparts. Part A has 20 items mainly concerning the participants’ preference for female vs male playmates, games, and toys in their childhood; the propensity for traditionally believed masculine household works; inquiry about fantasies in childhood, of common male or female sex-associated adult pursuits; and the frequency of frank cross-gender wishes at various ages. Part B has 9 items and consists mostly of items concerning cross-dressing and erotic desires presupposing homosexuality. It takes 15 minutes for the full completion and has good reliability and validity.
Scales for Sexual Orientation
Sexual orientation specifies the sexual attraction of a person toward people of different genders. This is often ignored while evaluating a person presenting sexual problems in a heterosexual relationship. Scales that have been developed to assess sexual orientation include Kinsey Scale, Klien Sexual Orientation Grid (KSOG), Lesbian, Gay, and Bisexual Identity Scale (LGBIS), Multidimensional Scale of Sexuality (MSS), and Dual Sexual Orientation Scales (DSOS).
Kinsey Scale: Kinsey homosexual-heterosexual scale was first designed by Alfred Kinsey to classify homosexual and heterosexual behavior. It assesses both sexual fantasies as well as overt sexual behavior. It uses 6 categories (0-6) to classify sexual orientation on a continuum from exclusively heterosexual to exclusively homosexual plus an additional category labeled X (no sociosexual contacts or reactions). The measurement of sexual behavior is relative to the subject’s total number of sexual incidents and not the absolute number of sexual incidents with the same sex.
Klein Sexual Orientation Grid (KSOG): It was developed by Fritz Klein as a further improvement of the Kinsey Scale. As per this scale, a person is rated across 7 areas, namely self-identification, sexual fantasies, sexual attraction, sexual behavior, emotional preference, social preference, and heterosexual-/gay lifestyle.
Lesbian, Gay, and Bisexual Identity Scale (LGBIS): It has 27 items and was designed to examine 8 areas of lesbian, gay, and bisexual (LGB) identity. It was developed by Mohr and Kendra in 2011. It comprises 8 subscales, namely concealment motivation, identity uncertainty, acceptance concerns, internalized homonegativity, difficult process, identity centrality, identity affirmation, and identity superiority. It has good internal consistency and test-retest reliability.
Multidimensional Scale of Sexuality (MSS): This scale assesses sexual orientation in the following categories, heterosexual, heterosexual with some homosexuality, concurrent bisexual, sequential bisexual, homosexual with some heterosexuality, past heterosexual, currently homosexual, past homosexual but currently heterosexual, homosexual, and asexual. It has 5 subscales (sexual behavior, arousal to erotic material, sexual attraction, emotional factors, and sexual dreams and fantasies), each with 9 items making a total of 45 items. Cronbach’s α scores across all the categories are 0.63 to 0.87.
Dual Sexual Orientation Scales (DSOS): This scale consists of 10 questions and it separates attraction to men from attraction to women on multiple sexual orientation dimensions (eg, romantic desires, emotional closeness, and fantasies). Each question requires the person to given information about attraction ratings on attraction to men and attraction to women on two 100-point subscales, for a total of 20 items. DSOS also predicts preferred relationships, traditional sexual orientation, identity labels, and childhood gender/sex-typed behavior, which supports the validity of the measure. It has good internal consistency and validity.
Scales Assessing Multiple Domains of Sexual Dysfunction
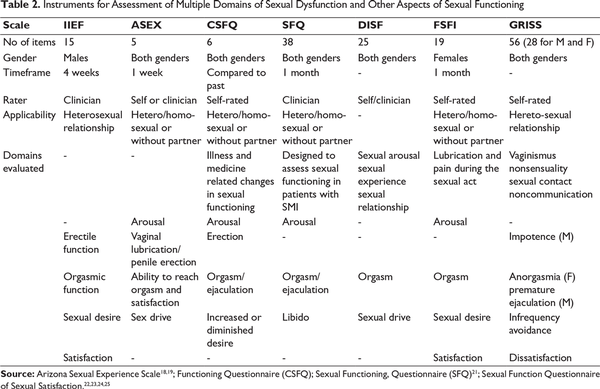
Adequate sexual functioning is a psychophysiological response and is considered to have 4 different phases, ie, desire (libido), arousal (excitement), orgasm, and resolution. The sexual response cycle is the basis for defining sexual dysfunction in subjects of either gender. Accordingly, various scales have been designed to assess sexual dysfunction related to the specific phase of the sexual response cycle or which evaluates the dysfunction in all the phases of the sexual response cycle. Clinicians and researchers have to choose various scales depending on the feasibility and the requirement. Some of the commonly used scales, for assessment of dysfunction in multiple domains of sexual response cycle, include Arizona Sexual Experience Scale (ASEX), International Index of Erectile Dysfunction (IIEF), Change in Sexual Functioning Questionnaire (CSFQ), Sexual Functioning Questionnaire (SFQ), Sexual Function Questionnaire, Female Sexual Function Index (FSFI), Derogatis Interview for Sexual Functioning (DISF), and Golombok-Rust Inventory of Sexual Satisfaction (GRISS) (Table 2).
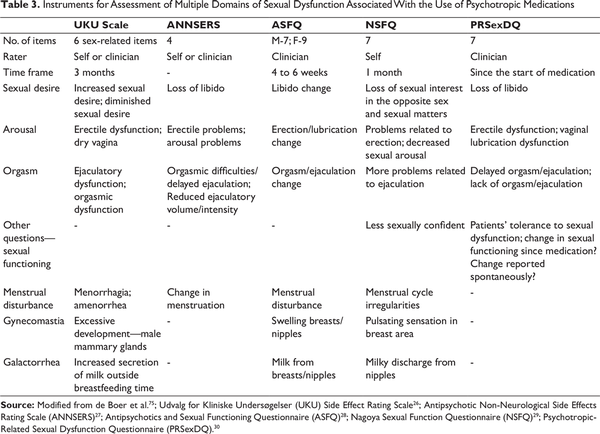
Many medications like various psychotropic drugs or antihypertensive drugs are associated with poor sexual functioning in various domains. Accordingly, some of the scales have been developed to specifically assess sexual dysfunction in multiple domains associated with the use of psychotropic medications. These include Udvalg for Kliniske Undersøgelser (UKU) Side Effect Rating Scale, Antipsychotic Non-Neurological Side Effects Rating Scale (ANNSERS), Antipsychotics and Sexual Functioning Questionnaire (ASFQ), Nagoya Sexual Function Questionnaire (NSFQ), and Psychotropic-Related Sexual Dysfunction Questionnaire (PRSexDQ). These scales have been reviewed in detail by de Boer et al. Interested readers can go through this review to have a better understanding of these scales.
Arizona Sexual Experience Scale (ASEX): This is a 5-item rating scale that evaluates the 4 phases of sexual functioning and 1 item assesses satisfaction with orgasm, ie, sexual drive, arousal with sexual stimuli, vaginal lubrication/penile erection, the ability to reach orgasm and the satisfaction with orgasm. Total score ranges from 5 to 30, with a score of 19 or more suggestive of sexual dysfunction. For individual domains, scores of 4 or 5 are considered as indicative of sexual dysfunction in that domain. It can be used in both the genders and is available as both clinician and self-rated scale. It has good convergent and discriminant validity along with internal consistency, test-retest reliability. It has been translated in many different languages including Hindi.
International Index of Erectile Dysfunction (IIEF): This is a 15-item validated questionnaire that was developed with aid from the pharmaceutical industry for the clinical research program of PDE5 inhibitor, sildenafil. It is a clinician-rated instrument applicable only for males and assesses sexual dysfunction over the last 4 weeks. It assesses five domains of sexual functioning, namely erectile functioning, orgasmic functioning, sexual desire, satisfaction with sexual intercourse, and overall satisfaction with the sexual act. It has a high degree of internal consistency for all the 5 domains and a complete scale (Cronbach’s α ≥0.73 and ≥0.91, respectively).
Change in Sexual Functioning Questionnaire (CSFQ): It is a 14-items structured interview/questionnaire, which compares sexual functioning with the past before a specific event like an illness or starting of medication, etc. It has 2 separate versions, one for males and another for females. It assesses erectile dysfunction, vaginal lubrication status, dysfunction in orgasm and ejaculation, increase or decrease in desire and frequency, and intensity of sexual contact. Concurrent validity is established, and test-retest reliability of the scale is high.
Sexual Functioning Questionnaire (SFQ): This is 38-items, the clinician-rated scale assessing sexual dysfunction over the last 1 month. It is specifically designed to measure the sexual functioning in patients suffering from severe mental illnesses (SMI). It assesses sexual functioning in the domains of libido, sexual arousal (erection in males, lubrication of vagina in females), masturbation, orgasm, and ejaculation. The scale has high reliability and internal consistency (Cronbach’s α 0.852) and has been validated in India too.
Sexual Function Questionnaire: This is a 34-items questionnaire, which is designed for assessing sexual dysfunction specifically in females. It evaluates 2 subtypes of sexual arousal—“arousal lubrication” and “arousal-sensation,” which are considered essential components for the assessment of Female Sexual Arousal Disorder (FSAD). Additionally, it assesses 7 domains of sexual functioning in females: sexual desire, physical arousal-sensation, physical arousal-lubrication, enjoyment, orgasm, pain, and partner relationship. A new version is also available named, SFQ-28, which has 28 items with high convergent validity, known group validity and high internal consistency (Cronbach’s α—from 0.70 to 0.93 for subjects with FSAD and HSDD).
Female Sexual Function Index (FSFI): This is a brief, 19-item self-report instrument for the assessment of female sexual function. It assesses 6 domains of sexual functioning, ie, desire (2 items), arousal (4 items), lubrication (4 items), orgasm (3 items), satisfaction (3 items), and pain (3 items). It has high test-retest reliability for each domain (r = 0.79 to 0.86), high internal consistency (Cronbach’s α values of 0.82 and higher), and good construct validity.
Derogatis Interview for Sexual Functioning (DISF): This is a brief, gender-based, multidimensional rating instrument designed to measure the quality of sexual functioning. It can be self-rated and clinician-rated and is used to measure 5 domains of sexual function: sexual fantasy, quality of experience, sexual arousal, sexual orgasm, and sexual drive. It has 25 items applicable for both the genders. A total of 5 items, 1 item for assessment of each of the following, ie, sexual cognition and fantasy, sexual arousal and sexual behavior, and experience domains; 6 items for assessment of sexual orgasm domain; and 4 items for assessment of sexual drive and sexual relationship domain. Internal consistency coefficients (Cronbach’s α—0.70 to 0.80) and test-retest coefficients (0.80 and 0.90) for the scale are high.
Golombok-Rust Inventory of Sexual Satisfaction (GRISS): This is a brief 28-item questionnaire for the assessment of sexual problems in heterosexual couples. It provides separate final scores for the quality of sexual functioning within a relationship for males and females separately. It is a good measure of the change in sexual function during the therapy. Its subscales measure and are highly fruitful in identifying impotence, PME, anorgasmia, vaginismus as well as in frequency, female avoidance, male and female dissatisfaction from the sexual act. It has reasonable reliability and validity.
Udvalg for Kliniske Undersøgelser (UKU) Side Effect Rating Scale: This is a generic scale to assess side effects with various medications. In terms of side effects, besides evaluating other side effects, one of the subscales evaluates the sexual side effects associated with medications. The 6 items of the scales that evaluate sexual dysfunction include increased sexual desire, diminished sexual desire, erectile dysfunction, ejaculatory dysfunction, orgasmic dysfunction, and dry vagina. It is both self- and clinician-rated and specifically asks about sexual dysfunction after the starting of psychotropic medication. Another advantage of this scale is that it also assesses gynecomastia, menorrhagia, amenorrhoea, and galactorrhoea. It has got good internal consistency, validity as well as reliability.
Antipsychotic Non-Neurological Side Effects Rating Scale (ANNSERS): This is also a generic scale to assess side effects associated with psychotropic drugs and besides evaluating other side effects also covers the assessment of sexual dysfunction. It a self- or clinician-rated scale, and the sexual dysfunction is assessed as loss of libido, increased libido, problems with sexual arousal, erectile difficulties/orgasmic difficulties, delayed ejaculation, reduction in ejaculation volume/intensity, and change in menstruation. Each of the items is rated on a 4-point scale.
Antipsychotics and Sexual Functioning Questionnaire (ASFQ): This is a 7- (for males) to 9-item (for female) clinician-rated scale assessing change in libido, lubrication, and erection. It also takes note of a change in orgasm, ejaculation, and menstrual disturbances over the last 4 to 6 weeks in patients receiving antipsychotic medications.
Nagoya Sexual Function Questionnaire (NSFQ): This is a 7-item self-rated questionnaire for the assessment of sexual functioning. It covers various domains of sexual functioning over the last 1 month in patients with schizophrenia who are taking antipsychotic drugs. It assesses sexual interest, erection, arousal, ejaculation, menstrual cycle irregularities, etc. It shows excellent internal consistency and strong test-retest reliability.
Psychotropic-Related Sexual Dysfunction Questionnaire (PRSexDQ): It is a 7-item clinician-rated scale assessing the sexual functioning since the start of antipsychotic medications. It can be used in both genders and assesses libido, erection, lubrication in females, orgasm, ejaculation, and any other change in sexual functioning after starting an antipsychotic drug. This questionnaire shows reasonable convergent validity and sensitivity for monitoring of changes in the sexual functions of a patient.
Udvalg for Kliniske Undersøgelser (UKU) Side Effect Rating Scale; Antipsychotic Non-Neurological Side Effects Rating Scale (ANNSERS); Antipsychotics and Sexual Functioning Questionnaire (ASFQ); Nagoya Sexual Function Questionnaire (NSFQ); Psychotropic-Related Sexual Dysfunction Questionnaire (PRSexDQ)
Scales for Sexual Desire
Sexual desire or libido is defined as “the sum of the forces that leads us toward and pushes us away from sexual behavior.” It can be an unnoticed cause of sexual dysfunction as a clinician can often assume sexual libido to be normal for the patient wanting treatment for sexual dysfunction. Scales that are specifically designed to assess sexual desire include Decreased Sexual Desire Screener (DSDS), Hurlbert Index of Sexual Desire (HISD), and Sexual Desire Inventory (SDI).
Decreased Sexual Desire Screener (DSDS): This is a short instrument that helps in diagnosing generalized or acquired, HSDD in adult women. DSDS was developed for physicians who do not specialize in diagnosis or management of female sexual dysfunction, for the diagnosis of generalized acquired HSDD in women. It consists of four “Yes” or “No” questions. Its validity has been evaluated and confirmed, ie, it has a sensitivity of 83.6% and specificity of 87.8%. In the cited study, it was found to be understood by 85.4% (76/89) of the included clinicians.
Hurlbert Index of Sexual Desire (HISD): It was developed by Apt and Hurlbert in 1992. It consists of 25 questions related to sexual desire, with a scoring system of 0 (all of the time) to +4 (never) out of which 13 items are reverse scored.
Sexual Desire Inventory (SDI): It is a self-rated scale developed to measure sexual desire over the last 1 month. It consists of 14 items with a different scoring for dyadic subscale (items: 1-8) and solitary subscale (items: 9-11). It takes about 5 minutes to complete. It has good internal consistency and test-retest reliability. Internal consistency measured by Cronbach’s α for the dyadic subscale (r = 0.86) and solitary subscale (r = 0.96) indicated strong reliability. The validity of scales is high.
Scales for Sexual Arousal/Erection
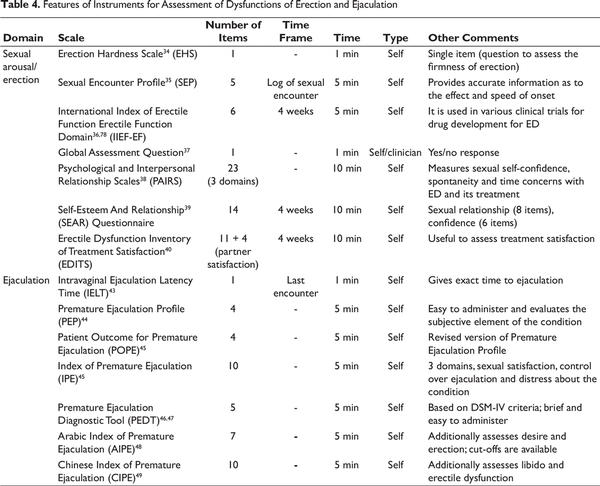
Sexual arousal or penile erection is the process of erection or strengthening of penile tissue during the process of sexual stimulation (physical or psychological). It is one of the most common causes of sexual dysfunction in males. Various instruments are available to assess erectile dysfunction (Table 4). These include the following.
International Index of Erectile Function Erectile Function Domain (IIEF-EF), : It consists of the first 5 questions of IIEF. It served as the standard tool for categorization of the severity of erectile dysfunction as reported by patients included in various clinical trials. The IIEF-EF domain is currently used in all clinical trials for the development of new erectile dysfunction medications. The rating of this scale is taken from patients’ recall of their sexual experience during the last 4 weeks period. The maximum score that can be reached in the IIEF-EF domain is 30 and the severity of ED is categorized as severe ED (score of 1-10), moderate ED (score of 11-17), mild ED (score of 18-25), and no ED or normal function (score of 26-30). All patients with an IIEF-EF domain score <26 are considered to have some degree of erectile dysfunction and therefore are generally included in most clinical trials on ED patients.
Erection Hardness Scale (EHS): This is a self-report single-item measure that is used to rate the hardness of a penile erection on a 5-point Likert scale ranging from 0 (penis do not enlarge) to 5 (the penis is completely hard and fully rigid). This scale has good test-retest reliability, quality, and distribution of responses, known-groups validity against the IIEF and is a good measure to see treatment responsiveness in clinical trials for drug development.
Sexual Encounter Profile (SEP): This is a log diary that is maintained by patients after each sexual intercourse attempt. It provides information regarding whether the erection was hard enough for vaginal penetration (SEP 2), or whether penile erection was maintained for completion of the sexual act (SEP 3) or a satisfactory sexual experience (SEP 4). This scale provides accurate information regarding the precise effect and speed of onset. It is mainly used for research purposes rather than clinical settings as it is time-consuming.
Global Assessment Question: This has also been used in various clinical trials of treatment for erectile dysfunction. It is a yes/no response in reply to the question, “Has the treatment you have been taking over the past 4 weeks improved your erections?” (Participant is supposed to compare their current erections after treatment with their erections before starting of treatment.)
Psychological and Interpersonal Relationship Scales (PAIRS): This is a self-rated instrument, which was developed to examine the overall psychological and interpersonal variables associated with ED and its treatment. It consists of 23 items and measures 3 domains, sexual self-confidence, spontaneity, and time concerns. The scale has good internal consistency, test-retest reliability, and divergent and convergent validity. A 15-item validated short form (SF-PAIRS) of this scale is also available.
Self-Esteem And Relationship (SEAR) Questionnaire: This is a patient-reported instrument that has 14 items that assess erection over the last 4 weeks. It provides information about 2 domains: sexual relationship (comprising of 8 items) and confidence (comprising of 6 items). The confidence domain is further divided into self-esteem (4 items) and an overall relationship (2 items). The scale has excellent psychometric properties, ie, it has good validity and reliability for measuring sexual relationship and self-esteem of patients with ED.
Erectile Dysfunction Inventory of Treatment Satisfaction (EDITS): This scale is used to examine the treatment satisfaction of the patient with ED and their partner. It is a self-administered scale that assesses erectile function over the last 4 weeks. It has 11 items for the patient version and additional 4 items for the partner version. It has good reliability and validity.
Scales for Sexual Orgasm
Orgasm is a transient peak sensation of immense pleasure, creating an altered state of responsiveness usually with induction of well-being and contentment. A poor orgasm can result in nonsatisfactory sex, resulting in poor sexual drive, and ultimately sexual dysfunction. Scales that can be used to assess problems related to orgasm include the following:
Orgasm Rating Scale (ORS): This scale uses a multidimensional approach to assess and quantify the psychological experience of orgasm in both men and women. ORS is a 40-item, self-report adjective-rating scale. A total of 2 subscales assess sensory and cognitive-affective dimensions, reflecting a 2-dimensional model of the psychological experience of orgasm that has been previously theorized and/or investigated. It describes the orgasm experiences attained under 2 sexual-context conditions: solitary masturbation and sex with a partner. ORS requires approximately 5 to 10 minutes to rate the 40 adjectives. It has got high internal consistency (Cronbach’s α—0.88-0.92) and validity.
Female Orgasm Scale: This assesses the consistency of female orgasm during partnered sexual activities (eg, intercourse, oral stimulation, self-stimulation with partner present) and overall satisfaction with orgasm frequency and quality. The scale comprises of 7 items. Five items inquire about the frequency of orgasm during different sexual activities: (a) intercourse, (b) intercourse with additional direct clitoral stimulation, (c) hand/manual stimulation of the clitoris and/or genitals by a partner, (d) self-stimulation of the clitoris and/or genitals in the presence of a partner, and (e) oral stimulation. Scale requires 2 to 5 minutes for completion. It has got high internal consistency (Cronbach’s α—0.84-0.86) and validity.
Scales for Assessment of Ejaculatory Dysfunction
Ejaculation of semen is usually the second to end-stage of the sexual cycle followed by residual stage. Problems in this stage are one of the most troubling and shameful for a man. “PME is defined as ejaculation that always or nearly always occurs before or within about 1 minute of vaginal penetration from the first sexual experience (lifelong PE) or a clinically significant and bothersome reduction in latency time, often to about 3 minutes or less (acquired PE),” as per International Society of Sexual Medicine. However, in recent times, the Diagnostic and Statistical Manual, 5th Revision (DSM-5) has changed the definition of PME. DSM-5 defines sexual dysfunction as “experience of a pattern of ejaculation occurring during partnered sexual activity within 1 minute after vaginal penetration and before the individual wishes it in almost all or all (75%-100%) sexual activity. Further, it specifies that the duration of symptoms should be of at least 6 months, symptoms must lead to significant distress and the dysfunction should not be explained by non-sexual mental disorder, a medication condition, use of drugs or medication or severe relationship distress or significant stressors.”
Depending upon the time taken for ejaculation after vaginal penetration, PME is categorized as mild (30 seconds to 1 minute), moderate (15-30 seconds) and severe (less than 15 seconds). Further depending on the duration of PME it can be categorized as lifelong or acquired and based on context, it is categorized as generalized (not limited to certain types of stimulation, situations, or partners) or situational (limited to specific types of stimulation, situations, or partners). Various scales/techniques that have designed to assess PME include the following (Table 4):
Intravaginal Ejaculation Latency Time (IELT): This is defined as the time between the start of vaginal intercourse and the starting of intravaginal ejaculation. It is a stopwatch technique and can be cumbersome for most of the patients. Prospective and retrospective measurements vary significantly and the latter is unreliable.
Premature Ejaculation Profile (PEP): This is a 4-item questionnaire enquiring about the patient’s subjective sense of control over ejaculation, distress associated with PME, interpersonal problems, and satisfaction levels with the sexual act. Each question is answered on a 5-point Likert scale and a score is calculated by taking a mean of the responses to all the 4 questions. It is a short scale and is easy to apply and evaluates the subjective element of the condition. The scale has good test-retest reliability and known groups’ validity.
Patient Outcome for Premature Ejaculation (POPE): This is a revised version of PEP. It also has 4 items, and it modifies the wording of the distress question and the rest of the 3 other questions are the same.
Index of Premature Ejaculation (IPE): It is a 10-item tool to measure control, satisfaction and distress in men with PE. It has 3 domains, namely control over ejaculation, sexual satisfaction, and distress about the condition. Each of the 3 domains contains various questions that help in assessing a more vast aspect of the condition as compared to the single item domains of the PEP scale. It has good test-retest reliability and internal consistency.
Premature Ejaculation Diagnostic Tool (PEDT), : This is a 5-item tool that was developed based on DSM IV-TR criteria of PE. The PEDT is better used as a screening measure for PE rather than a measure of assessment of the impact of an intervention. By employing a 3-level cut-off score it labels the construct as a diagnosis of PE (≤8), possible PE (9-10), and no PE (≥11). It can be completed by patients easily within a brief period and presents to the clinicians a reliable (Cronbach α—0.77) and valid assessment of PE status.
Arabic Index of Premature Ejaculation (AIPE): This is a 7-item tool for assessment of any ejaculation abnormality. It additionally assesses sexual desire and penile erection as well. The main assessment involves time to ejaculation, difficulty in prolonging ejaculation during the sexual act, satisfaction level with sexual intercourse, and personal distress with the ejaculation problem. A cut-off score of 30 (range of scores 7-35) warrants a diagnosis of PME with a sensitivity score of 0.98 with a specificity score of 0.88.
Chinese Index of Premature Ejaculation (CIPE): This has 10 questions that focus on sexual libido, erectile functioning, ejaculatory latency, sexual satisfaction with the overall act, difficulty in delaying ejaculation, self-confidence, and depression. Each item/question is to be responded to on a 5-point Likert scale. This scale has got a high sensitivity and specificity of 97.6% and 94.74%, respectively. Patients with PE can be divided into 3 groups based on their total score, ie, severe (total score <9 points), moderate (10-14 points), and mild ( >15 points).
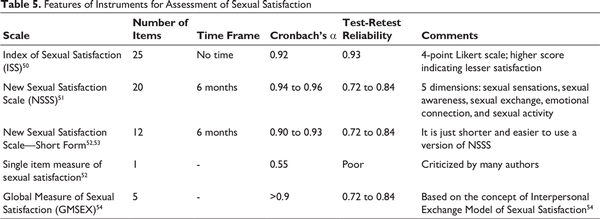
Scales for Assessment of Sexual Satisfaction
Sexual satisfaction is a subjective feeling and is considered as an important parameter to indicate sexual health. It is reported to strongly correlate with satisfaction with the relationship with the partner. Various scales have been designed to assess sexual satisfaction (Table 5).
Index of Sexual Satisfaction (ISS): This is brief self-rated scale designed to measure the degree of dissatisfaction in the sexual aspect of a dyadic relationship. It has 25 items each item rated on a 4-point Likert scale, which can be completed in 5 to 7 minutes. The obtained score ranges from 0 to 100 with a higher score indicating lesser satisfaction. It is a reliable scale with Cronbach’s α value of 0.92 and a validity coefficient of 0.76.
New Sexual Satisfaction Scale (NSSS): It is a scale whose framework is derived from psychotherapy literature and comprises 5 dimensions, ie, sexual sensations, sexual presence/awareness, sexual exchange, emotional connection/closeness, and sexual activity. It contains 20 items and measures sex life during the past 6 months and rating is supposed to be done on a 5-point Likert scale. The full scale takes 5 minutes to complete. The higher the score more is sexual satisfaction. Internal consistency of the scale has been reported to be good with Cronbach’s α = 0.94 to 0.96 for the full-scale and 0.91 to 0.93 and 0.90 to 0.94 for both subscales.
New Sexual Satisfaction Scale—Short Form (NSS-SF), : This scale was developed to facilitate the use of the NSSS in clinical and nonclinical studies. It is a short version of NSSS, comprises of 12 items. The internal consistency of the short version is good (Cronbach’s α = 0.90-0.93). It also has good test-retest reliability and validity.
Single Item Measure of Sexual Satisfaction: This is a 1-item scale with a 5-point rating on a Likert scale. It has got an average internal consistency value of 0.55 and is reported to have relatively poor test-retest reliability. Many authors have criticized the use of the single item for measurement for the assessment of any construct.,
Global Measure of Sexual Satisfaction (GMSEX): This measures global sexual satisfaction in the context of an intimate relationship. It is based on the theoretical concept of the Interpersonal Exchange Model of Sexual Satisfaction (IEMSS). It has got 5 items, rated on a 7-point rating scale (good-bad, pleasant-unpleasant, positive-negative, satisfying-unsatisfying, and valuable-worthless), with the baseline question of “In general, how would you describe your sexual relationship with your partner?” It has shown to have a high degree of internal consistency with Cronbach’s α >0.90 in individuals in long-term relationships and test-retest reliability of 0.78 to 0.84 at 2 weeks to 3 months of follow up.
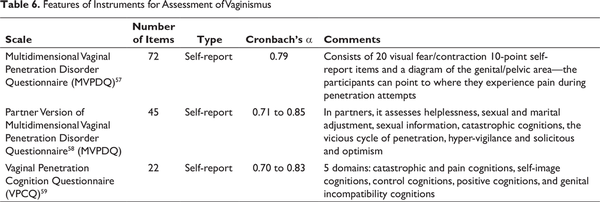
Rating Scales Specifically for Vaginismus
Vaginismus or genito-pelvic pain/penetration disorder refers to 4 commonly comorbid symptom dimensions, including difficulty in having intercourse, genito-pelvic pain, fear of pain or vaginal penetration, and tension of the pelvic floor muscles. It is associated with dysfunction in the sexual domain of patient life as well as the partner. Following scales can be used for assessment of vaginismus (Table 6).
Multidimensional Vaginal Penetration Disorder Questionnaire (MVPDQ): This is a 72-item, a self-administered questionnaire that consists of 20 visual fear/contraction 10-point self-report items and a diagram of genital/pelvic area so that the participants could point to where they experience pain during penetration attempts. It assesses the following domains: (1) catastrophic cognitions and fears regarding vaginal penetration, (2) pelvic muscle dysfunction and pain during penetration attempts, (3) psychological and relational problems experienced by women when vaginal penetration fails, (4) sexual information about penetration and female and male genital anatomy, (5) hyper-vigilance and avoidance during vaginal penetration attempts, (6) marital adjustment, (7) optimism and positive cognitions regarding future and treatment, (8) penetration motivation, and (9) negative thoughts about genital compatibility. Intensity of pain is assessed on a 4-point scale (0 = no pain, 1 = some pain, 2 = moderate pain, 3 = severe pain). Cronbach’s α value for the whole scale is 0.79 and the test-retest values ranging from 0.78 to 0.87 indicates that MVPDQ subscales have appropriate levels of stability over 2 weeks.
Partner Version of Multidimensional Vaginal Penetration Disorder Questionnaire (MVPDQ): This is a 45-item, self-reporting questionnaire, with 5-point rating on a Likert scale (1 being never to 5 being always), except for marital intimacy that is a 10-point rating Likert scale. Cognitions, sexual and marital relations related to vaginal penetration in spouses of females with vaginismus can be assessed with this instrument. It assesses the following domains, related to vaginismus, ie, helplessness, sexual and marital adjustment, sexual information, catastrophic cognitions, the vicious cycle of penetration, hyper-vigilance, and solicitous and optimism.
Vaginal Penetration Cognition Questionnaire (VPCQ): This is a 22-item, self-reported questionnaire. It has 5 domains, namely catastrophic and pain cognitions, self-image cognitions, control cognitions, positive cognitions, and genital incompatibility cognitions. The reliability of these 5 subscales ranges from 0.70 to 0.83 with test-retest reliability being average. For assessment of cognitions related to vaginal penetration in women with vaginismus, VPCQ is considered to be a valid and reliable brief self-report measure.
Scales for Assessment of Sexual Quality of Life
It is a known fact that poor sexual life is associated with a poorer overall quality of life (QOL). Poor quality of sexual life may be associated with poor sexual functioning and should be assessed thoroughly. Various scales have been developed to assess the sexual quality of life. These are discussed as follows.
Quality of Sexual Life Questionnaire (QVS): This is used to assess the quality of life in patients suffering from erectile dysfunction. This questionnaire comprises of 27 items. It is divided into 3 subscales regarding the sexual life of the patient, skills and psychosocial well-being of the patient. One score per subscale is calculated giving a total of 4 scores and 1 global index grouping items from sexual life and psychological well-being. The total score ranges from 0 (poor quality of life) to 100 (good quality of life). It has good reliability and validity with internal consistency values being 0.87, 0.91, and 0.78 for sexual life, skills, and psychosocial well-being items, respectively.
Sexual Life Quality Questionnaire (SLQQ): This scale evaluates the QOL in the sexual domain of life and satisfaction with treatments for erectile dysfunction of the patients and their sexual companions. Out of a total of 16 items, 10 items deal with the area of sexual QOL that can be seen as a summated sexual QOL scale measure. The remaining 6 items comprise a scale measuring the area of satisfaction with treatment for ED. The latter measurement is a fair indicator of treatment preference. Cronbach’s α for the summated QOL scale is 0.94 and for satisfaction with treatments for erectile dysfunction is 0.92.
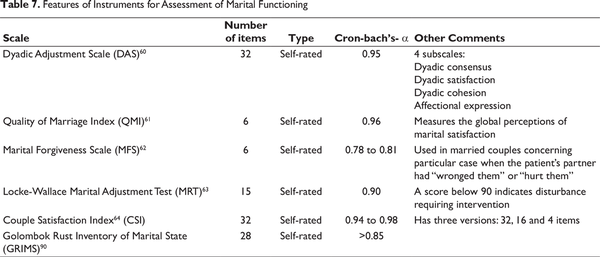
Rating Scales for Marital/Couple Functioning
Marital functioning means that how satisfied a person is in his married life in interpersonal, economic, personal, and sexual domains. It is a known fact that sexual dysfunction can lead to significant marital dysfunction and vice-versa. Accordingly, it is very important to assess the marital functioning in the patient presenting with sexual dysfunction to have a better understanding of the problem in the relationship domain. Various scales have been developed to assess marital functioning (Table 7). Some of the commonly used scales include the following.
Dyadic Adjustment Scale (DAS): This is the 32-items scale to measure the quality of a relationship. It consists of 4 subscales: Dyadic consensus (which is the measurement of the degree to which participant agrees with their partner), dyadic satisfaction (which is the measurement of the degree of satisfaction with the partner), dyadic cohesion (which is the measurement of the degree of participation of respondent and partner in activities together), and affectional expression (which is the measurement of the degree to which respondent agrees with partner concerning emotional affection). Cronbach’s α for the above scale ranges from 0.7 (for the subscale of affectional expression) to 0.95 (for the complete scale). DAS and its 4 subscales have a good level of internal consistency.
Quality of Marriage Index (QMI): This is a brief, self-administered questionnaire that measures the global perceptions of marital satisfaction. It is a brief 6 items questionnaire that is a reliable and valid measure for assessing the overall marital satisfaction in patients suffering from infertility. It has an excellent psychometric profile and gives a better and more reliable measure for longer term relationships.
Marital Forgiveness Scale (MFS): This is the measure for forgiveness in the marital context. This scale is used in married couples about particular case when the patient’s partner had “wronged them” or “hurt them.” Greater agreement with statements in the scales means higher scores. Cronbach’s α value for the scale has been reported to be good for both positive dimension (for wives = 0.79, husbands = 0.78) and negative dimension (for wives = 0.81 and husbands = 0.78).
Locke-Wallace Marital Adjustment Test (MRT): This is a 15-item scale used to evaluate marital adjustment in married couples. Low scores indicate dissatisfaction and high scores indicate higher satisfaction in the marital life. A score below 90 indicates a disturbance. It has got split-half reliability of 0.90 and discriminant and concurrent validity of 0.89.
Couple Satisfaction Index (CSI): This scale has multiple versions (32-item, 16 items, and 4 items) to measure one’s satisfaction in a relationship. The scale has a variety of items with different response scales and formats. This scale has good psychometric properties.
Golombok Rust Inventory of Marital State (GRIMS): A 28-item questionnaire that evaluates the quality of the relationship between a married couple or a couple in a live-in relationship. It is considered being sensitive to picking up change in a relationship over time. It is considered as a companion questionnaire to GRISS, which is used to assess the sexual functioning during sex therapy.
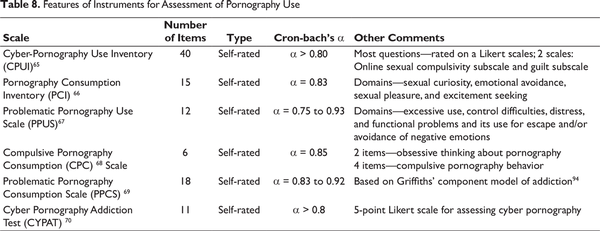
Rating Scales for Pornography Use
Though difficult to define, most authors would agree that pornography contains sexually explicit material depicting naked or seminaked bodies engaged in genital stimulation or sexual acts. It has been suggested that people who lack satisfying sexual relations may turn to pornography as a way to meet their sexual needs or explore stigmatized aspects of their sexuality. Further, at times, people may require viewing of pornography to get sexual stimulation. However, excessive use of pornography can also lead to a lack of interest in the partner and can lead to addiction in viewing the same. It is important to establish the use of pornography for a better understanding of the patient’s sexual interests and understanding. Various scales that have been developed to assess the use of pornography include the following (Table 8).
Cyber-Pornography Use Inventory (CPUI): This is a 40-item self-administered measure comprising of 6 assumed subscales (including compulsivity, social, isolated, interest, efforts, and guilt subscales). Most of the questions are rated on Likert scales ranging from never to always or strongly agree to strongly disagree. CPUI is meant to place high importance on the online sexual compulsivity subscale (high scores indicating of compulsive and addictive tendencies) and the guilt subscale (high scores indicating a high amount of guilt regarding internet pornography usage). The scale shows good reliability (α > 0.80) for each factor, as well as some measure of construct validity.
Pornography Consumption Inventory (PCI): It is an instrument that is designed to measure various motivations that lead to pornography use among males having hypersexuality. It has 15 items and assesses domains of sexual curiosity, emotional avoidance, sexual pleasure, and excitement seeking. It does not give any pornography consumption behavior related information; neither does it assess the compulsive nature of the aforementioned behavior. Cronbach’s α value for the overall scale (α = 0.83) is highly confirming and has a high internal consistency. The scale has modest evidence for convergent and divergent validity.
Problematic Pornography Use Scale (PPUS): This is a 12-item questionnaire covering 4 major domains including excessive use, control difficulties, distress, and functional problems and its use for escape and/or avoidance of negative emotions. It shows the high internal consistency, convergent validity, and construct validity with Cronbach’s α values for individual domains ranging from 0.75 to 0.93.
Compulsive Pornography Consumption (CPC) Scale: This includes 6 items and was devised to measure compulsive pornography use including 2 items assessing obsessive thinking about pornography and 4 items assessing compulsive pornography behavior. It assesses all the behavior during the previous 3 months. Participants respond on each item using a 7-point Likert scale, with a response range of 1 = “very frequently” to 7 = “never.” Cronbach’s α of the scale is reported to be 0.85.
Problematic Pornography Consumption Scale (PPCS): This is an 18-item self-rated questionnaire that assesses the problematic porn consumption in the previous 6 months and is based on Griffiths’ component model of addiction. All the questions are assessed on a Likert scale from 0 (never) to 7 (all the time). A final score of 76 or more indicates problematic pornography use. It has good reliability and internal consistency measures.
Cyber Pornography Addiction Test (CYPAT): This is a new, brief self-report screening scale. It has 11 items that are scored on a 5-point Likert scale for assessing cyber pornography. Cronbach’s α coefficient suggested excellent reliability. This scale also shows good construct, convergent, and divergent validity.
Discussion
Assessments of various dimensions of sexual functioning are important, both from the patient and the clinician’s perspective. Many a time, patient’s complaint about sexual dysfunction, for which they are distressed. At times they may not be aware or acknowledge many other aspects that may be affecting adequate sexual functioning. Accordingly, a thorough evaluation of various aspects of sexual functioning can broaden the understanding of the problem, for both the patient and the clinician. Rating scales provide a structured format to assess various dimensions of sexual functioning. Many of these rating scales are self-report questionnaires, which often help the patient is expressing themselves better, as many times people are shy about discussing their aspects during an interview situation. In terms of research, rating scales are at the core of any kind of quantitative study in psychiatry and are often considered as an equivalent of any kind of investigation report in any field of medicine. Rating scales improve the collection, synthesis, and reporting of information, ensure complete coverage of the relevant issue and help in categorization and/or quantifying the topic in hand.
Accordingly, clinicians should use various rating scales in routine clinical practice to improve the detection and monitoring of various aspects of sexual functioning. These measures can also provide an objective measure of the sexual functioning, for medico-legal purposes; however, it is important to remember that they are not as reliable as more valid biological tests. Further, it should be understood that the rating scales are not a substitute to a detailed history for diagnosis and assessment of the severity of any sexual problem. The rating scales should only be used as an add-on to a detailed history taking and clinical examination. A thorough history taking can be aided by the use of scale for assessment of sexual knowledge, marital functioning (if applicable) and scales for assessment of various phases of the sexual cycle. However, it is important to remember that clinicians should use gender-specific rating scales and use language-specific translated and validated scales for proper assessment. In terms of choosing the scales, an initial assessment can involve using a broad scale followed by a specific scale. A thorough evaluation should also take into account the partner’s opinion and partner-specific scales if available can be incorporated in the assessment. Further, while selecting scales, clinicians should preferably use group-specific scales, like while evaluating patients on certain treatment (example antipsychotics) and patients with SMI.
An important limitation of the existing scales is that most of these scales have not been validated across different cultures and have not been translated into different languages. Some of the scales that have been developed and or validated in the Indian context include SKAQ, DSQ, Scale for Assessment of Female Dhat syndrome (SAFED),, Dhat syndrome interview schedule, and Diagnostic and assessment instrument for Dhat syndrome. Among the various scales assessing sexual dysfunction, only SFQ has been validated in Indian patients. Some of the other scales that have been translated into Hindi include ASEX and IIEF.
In general, almost all the instruments have good psychometric properties in the form of reliability and validity. However, it is important to note that although researchers have evaluated the sensitivity, specificity, and inter-rater reliability of various measuring tools, there has been a significant difference in the methodology used for testing the aforementioned constructs. Another point to be noted is that most of the scales have been assessed for and validated in young subjects only and its validity in other age groups is not properly known. Research has not answered the ease of use of these instruments in various treatment settings by different types of professionals. Our literature review also suggests that many instruments have been evaluated only one time, ie, during the process of development and many of these instruments have not been used much in the research.
How to Select a Scale?
As most of the available scales have been validated, it is difficult to recommend the use of specific scales for the assessment of various aspects of sexual dysfunction. Accordingly, although in the following section, we make certain suggestions, for selection of scales, these suggestions should be considered as broad recommendations and the clinicians and researchers should choose scales, based on their needs, needs of the patient, and the time that can be afforded to complete the various scales.
In terms of choosing a scale for assessment of various sexual dimensions, if one wants to use a brief scale, having broad coverage of various dimensions, ASEX is a good brief instrument. However, a major limitation of this scale is that it does not provide any information about the various components of each sexual cycle stage. If someone wants to evaluate the sexual functioning in more detail, IIEF is considered to be a preferred scale for males and FSFI is a good scale for women. However, scales like GRISS can expand the assessment of various aspects of sexual functioning. If the aim of the evaluation is the assessment of ED only, then IIEF-EF is a good scale. However, in clinical practice, for broader assessment in the initial part of assessment PAIRS should be used to understand the psychological and relationship factors, which may be contributing to ED. While monitoring during therapy, combining SEP with IIEF-EF and EHS can provide much more useful information. For PME PEP or POPE may be preferred, because of the brevity. In terms of the sexual satisfaction scale, a single item satisfaction scale is often preferred, but this does not usually provide adequate information. The selection of scales like NSSS or its short form can provide broader information. In terms of vaginismus available scales assess different aspects of vaginismus and selection of the scale should accordingly be based on the specific aspect to be evaluated. In general, MVPDQ, although can be considered as a lengthy scale, but provides more comprehensive information. In terms of scales assessing the marital/couple functioning DAS has been quite frequently used in Indian studies, because of the availability of the Hindi version. However, QMI can be considered a brief measure, which also provides useful information. For evaluation of the Dhat syndrome DSQ can be used, as it comprehensively assesses various aspects of Dhat syndrome and is available in multiple languages. In terms of assessment of sexual knowledge, SKAQ has been most extensively used in clinical practice and research. For assessment of sexual orientation, KSOG is a brief scale, which assesses various dimensions of sexual orientation.
Conclusions
The rating of various dimensions of sexual functioning has advanced significantly in the last 3 decades. Instruments have been designed and tested for reliability and validity not only for common sexual problems like ED and PME but also for the assessment of newer and relatively less known conditions like hypoactive sexual desire and problematic pornography use. Gender-specific and language/population-specific scales have also been developed for the assessment of some of the aspects of sexual functioning. Along with that many scales are also available for assessing the sexual dysfunction associated with known factors like medication use and culturally specific phenomena like Dhat syndrome.
In the future, there is a need to revise some of these instruments and design more language-specific, easy to use, brief, and more informative scales. Further, there is a need to validate the available scales in different cultures and patients of different age groups.
Sandeep Grover
https://orcid.org/0000-0002-2714-2055
References
- 1. Lewis RW, Fugl-Meyer KS, Bosch R Epidemiology/risk factors of sexual dysfunction. J Sex Med. 2004; 1:35–39.
- 2. Rosen RC. Prevalence and risk factors of sexual dysfunction in men and women. Curr Psychiatry Rep. 2000; 2:189–195.
- 3. Avasthi AK, Varma VK, Nehra R, Das K. Construction and standardization of a sex knowledge and attitude questionnaire (SKAQ), in simple Hindi, for north Indian population. Indian J Psychiatry. 1992; 34:24–27.
- 4. McCabe MP, Cummins RA, Deeks AA. Construction and psychometric properties of sexuality scales: sex knowledge, experience, and needs scales for people with intellectual disabilities (SexKen-ID), people with physical disabilities (SexKen-PD), and the general population (SexKen-GP). Res Dev Disabil. 1999; 20:241–254.
- 5. Sharan P, Avasthi A, Gupta N, Mohanty M, Gill S, Jain A. Development of Dhat syndrome interview schedule. Indian J Psychiatry. 2003;88.
- 6. Grover S, Avasthi A, Aneja J Comprehensive questionnaire for assessment of Dhat syndrome: development and use in patient population. J Sex Med. 2014; 11:2485–2495.
- 7. Grover S, Kate N, Avasthi A, Rajpal N, Umamaheswari V. Females too suffer from Dhat syndrome: a case series and revisit of the concept. Indian J Psychiatry. 2014; 56:388–392.
- 8. Grover S, Avasthi A, Gupta S, Hazari N, Malhotra N. Do female patients with nonpathological vaginal discharge need the same evaluation as for Dhat syndrome in males. Indian J Psychiatry. 2016;58:61.
- 9. Prakash S, Sharan P, Sood M. A study on phenomenology of Dhat syndrome in men in a general medical setting. Indian J Psychiatry. 2016; 58:129–141.
- 10. Stern BB, Barak B, Gould SJ. Sexual identity scale: a new self-assessment measure. Sex Roles. 1987; 17:503–519.
- 11. Freund K, Nagler E, Langevin R, Zajac A, Steiner B. Measuring feminine gender identity in homosexual males. Arch Sex Behav. 1974; 3:249–260.
- 12. Blanchard R, Freund K. Measuring masculine gender identity in females. J Consult Clin Psychol. 1983; 51:205–214.
- 13. Kinsey AC, Pomeroy WB, Martin CE. Sexual behavior in the human male. J Clin Psychol. 2003; 6:894–898.
- 14. Klein F, Sepekoff B, Wolf TJ. Sexual orientation: a multi-variable dynamic process. J Homosex. 1985; 11:35–49.
- 15. Worthington RL, Dillon FR, Becker-Schutte AM. Development, reliability, and validity of the lesbian, gay, and bisexual knowledge and attitudes scale for heterosexuals (LGB-KASH). J Couns Psychol. 2005; 52:104–118.
- 16. Berkey BR, Perelman-Hall T, Kurdek LA. The multidimensional scale of sexuality. J Homosex. 1990; 19:67–87.
- 17. Hale A, Miller LB, Weaver J, Husney SQ, Henares R. The dual scales of sexual orientation. J Bisex. 2019;19(4):1–32.
- 18. McGahuey CA, Gelenberg AJ, Laukes CA The Arizona Sexual Experience Scale (ASEX): reliability and validity. J Sex Marital Ther. 2000; 26:25–40.
- 19. Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997; 49:822–830.
- 20. Clayton AH, McGarvey EL, Clavet GJ. The Changes in Sexual Functioning Questionnaire (CSFQ): development, reliability, and validity. Psychopharmacol Bull. 1997; 33:731–745.
- 21. Krishna K, Avasthi A, Grover S. Validation of sexual functioning questionnaire in Indian patients. Indian J Psychol Med. 2014;36:404.
- 22. Quirk FH, Heiman JR, Rosen RC, Laan E, Smith MD, Boolell M. Development of a sexual function questionnaire for clinical trials of female sexual dysfunction. J Womens Health Gend Based Med. 2002; 11:277–289.
- 23. Derogatis LR. The Derogatis Interview for Sexual Functioning (DISF/DISF-SR): an introductory report. J Sex Marital Ther. 1997; 23:291–304.
- 24. Rosen R, Brown C, Heiman J The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000; 26:191–208.
- 25. Rust J, Golombok S. The Golombok-Rust Inventory of Sexual Satisfaction (GRISS). Br J Clin Psychol. 1985;24(Pt 1):63–64.
- 26. Lingjaerde O, Ahlfors UG, Bech P, Dencker SJ, Elgen K. The UKU side effect rating scale. A new comprehensive rating scale for psychotropic drugs and a cross-sectional study of side effects in neuroleptic-treated patients. Acta Psychiatr Scand 1987;76(suppl 334):1–100.
- 27. Mahmoud A, Drake RJ, Lewis SW, Hayhurst KP, Barnes TRE. The ANNSERS (Antipsychotic Non-Neurological Side Effects Rating Scale): validation of sexual side-effect measurement. Ther Adv Psychopharmacol. 2011; 1:97–100.
- 28. de Boer MK, Castelein S, Bous J The Antipsychotics and Sexual Functioning Questionnaire (ASFQ): preliminary evidence for reliability and validity. Schizophr Res. 2013; 150:410–415.
- 29. Kikuchi T, Iwamoto K, Sasada K, Aleksic B, Yoshida K, Ozaki N. Reliability and validity of a new sexual function questionnaire (Nagoya Sexual Function Questionnaire) for schizophrenic patients taking antipsychotics. Hum Psychopharmacol. 2011; 26:300–306.
- 30. Montejo AL, Rico-Villademoros F. Psychometric properties of the Psychotropic-Related Sexual Dysfunction Questionnaire (PRSexDQ-SALSEX) in patients with schizophrenia and other psychotic disorders. J Sex Marital Ther. 2008; 34:227–239.
- 31. Clayton AH, Goldfischer ER, Goldstein I, Derogatis L, Lewis-D’Agostino DJ, Pyke R. Validation of the decreased sexual desire screener (DSDS): a brief diagnostic instrument for generalized acquired female hypoactive sexual desire disorder (HSDD). J Sex Med. 2009; 6:730–738.
- 32. Apt CV, Hurlbert DF. Motherhood and female sexuality beyond one year postpartum: a study of military wives. J Sex Educ Ther. 1992; 18:104–114.
- 33. Spector IP, Carey MP, Steinberg L. The sexual desire inventory: development, factor structure, and evidence of reliability. J Sex Marital Ther. 1996; 22:175–190.
- 34. Mulhall JP, Goldstein I, Bushmakin AG, Cappelleri JC, Hvidsten K. Validation of the erection hardness score. J Sex Med. 2007; 4:1626–1634.
- 35. Porst H, Padma-Nathan H, Giuliano F, Anglin G, Varanese L, Rosen R. Efficacy of tadalafil for the treatment of erectile dysfunction at 24 and 36 hours after dosing: a randomized controlled trial. Urology. 2003; 62:121–125–126; discussion 125–126.
- 36. Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999; 11:319–326.
- 37. Giuliano F, Rubio-Aurioles E, Kennelly M Vardenafil improves ejaculation success rates and self-confidence in men with erectile dysfunction due to spinal cord injury. Spine. 2008; 33:709–715.
- 38. Swindle RW, Cameron AE, Lockhart DC, Rosen RC. The psychological and interpersonal relationship scales: assessing psychological and relationship outcomes associated with erectile dysfunction and its treatment. Arch Sex Behav. 2004; 33:19–30.
- 39. Cappelleri JC, Althof SE, Siegel RL, Shpilsky A, Bell SS, Duttagupta S. Development and validation of the Self-Esteem And Relationship (SEAR) questionnaire in erectile dysfunction. Int J Impot Res. 2004; 16:30–38.
- 40. Althof SE, Corty EW, Levine SB EDITS: development of questionnaires for evaluating satisfaction with treatments for erectile dysfunction. Urology. 1999; 53:793–799.
- 41. Mah K, Binik YM. Do all orgasms feel alike? Evaluating a two-dimensional model of the orgasm experience across gender and sexual context. J Sex Res. 2002; 39:104–113.
- 42. Mcintyre-Smith A, Fisher WA. Female orgasm scale. In: Handbook of Sexuality-Related Measures. 3rd ed. New York, NY: Routledge; 2011.
- 43. Waldinger MD, Quinn P, Dilleen M, Mundayat R, Schweitzer DH, Boolell M. A multinational population survey of intravaginal ejaculation latency time. J Sex Med. 2005; 2:492–497.
- 44. Patrick DL, Giuliano F, Ho KF, Gagnon DD, McNulty P, Rothman M. The Premature Ejaculation Profile: validation of self-reported outcome measures for research and practice. BJU Int. 2009; 103:358–364.
- 45. Althof SE. Patient reported outcomes in the assessment of premature ejaculation. Transl Androl Urol. 2016; 5:470–474.
- 46. Y-P Huang, Chen B, Ping P The premature ejaculation diagnostic tool (PEDT): linguistic validity of the Chinese version. J Sex Med. 2014; 11:2232–2238.
- 47. Kam SC, Han DH, Lee SW. The diagnostic value of the premature ejaculation diagnostic tool and its association with intravaginal ejaculatory latency time. J Sex Med. 2011; 8:865–871.
- 48. Arafa M, Shamloul R. Development and evaluation of the Arabic Index of Premature Ejaculation (AIPE). J Sex Med. 2007; 4:1750–1756.
- 49. Y-M Yuan, Z-C Xin, Jiang H Sexual function of premature ejaculation patients assayed with Chinese Index of Premature Ejaculation. Asian J Androl. 2004; 6:121–126.
- 50. Hudson WW, Harrison DF, Crosscup PC. A short-form scale to measure sexual discord in dyadic relationships. J Sex Res. 1981; 17:157–174.
- 51. Stulhofer A, Busko V, Brouillard P. Development and bicultural validation of the new sexual satisfaction scale. J Sex Res. 2010; 47:257–268.
- 52. Mark KP, Herbenick D, Fortenberry JD, Sanders S, Reece M. A psychometric comparison of three scales and a single-item measure to assess sexual satisfaction. J Sex Res. 2014; 51:159–169.
- 53. Strizzi J, Fernández-Agis I, Alarcón-Rodríguez R, Parrón-Carreño T. Adaptation of the New Sexual Satisfaction Scale-Short Form into Spanish. J Sex Marital Ther. 2016; 42:579–588.
- 54. K-A Lawrance, Byers ES. Sexual satisfaction in long-term heterosexual relationships: the interpersonal exchange model of sexual satisfaction. Pers Relatsh. 1995; 2:267–285.
- 55. Costa P, Arnould B, Cour F Quality of Sexual Life Questionnaire (QVS): a reliable, sensitive and reproducible instrument to assess quality of life in subjects with erectile dysfunction. Int J Impot Res. 2003; 15:173–184.
- 56. Woodward JMB, Hass SL, Woodward PJ. Reliability and validity of the sexual life quality questionnaire (SLQQ). Qual Life Res. 2002; 11:365–377.
- 57. Molaeinezhad M, Roudsari RL, Yousefy A, Salehi M, Khoei EM. Development and validation of the multidimensional vaginal penetration disorder questionnaire (MVPDQ) for assessment of lifelong vaginismus in a sample of Iranian women. J Res Med Sci. 2014; 19:336–348.
- 58. Molaeinezhad M, Khoei EM, Salehi M, Yousfy A, Roudsari RL. Validation of the partner version of the multidimensional vaginal penetration disorder questionnaire: a tool for clinical assessment of lifelong vaginismus in a sample of Iranian population. J Educ Health Promot. 2014;3:114.
- 59. Klaassen M, TerKuile MM. Development and initial validation of the vaginal penetration cognition questionnaire (VPCQ) in a sample of women with vaginismus and dyspareunia. J Sex Med. 2009; 6:1617–1627.
- 60. Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J Marriage Fam. 1976; 38:15–28.
- 61. Norton R. Measuring marital quality: a critical look at the dependent variable. J Marriage Fam. 1983; 45:141–151.
- 62. Fincham FD, Beach SRH. Forgiveness in marriage: implications for psychological aggression and constructive communication. Pers Relatsh. 2002; 9:239–251.
- 63. Locke HJ, Wallace KM. Short marital-adjustment and prediction tests: their reliability and validity. Marriage Fam Living. 1959; 21:251–255.
- 64. Funk JL, Rogge RD. Testing the ruler with item response theory: increasing precision of measurement for relationship satisfaction with the Couples Satisfaction Index. J Fam Psychol. 2007; 21:572–583.
- 65. Grubbs JB, Sessoms J, Wheeler DM, Volk F. The cyber-pornography use inventory: The development of a new assessment instrument. Sex Addict Compuls. 2010; 17:106–126.
- 66. Reid RC, Li DS, Gilliland R, Stein JA, Fong T. Reliability, validity, and psychometric development of the pornography consumption inventory in a sample of hypersexual men. J Sex Marital Ther. 2011; 37:359–385.
- 67. Kor A, Zilcha-Mano S, Fogel YA, Mikulincer M, Reid RC, Potenza MN. Psychometric development of the Problematic Pornography Use Scale. Addict Behav. 2014; 39:861–868.
- 68. Noor SW, Simon Rosser BR, Erickson DJ. A brief scale to measure problematic sexually explicit media consumption: psychometric properties of the Compulsive Pornography Consumption (CPC) Scale among men who have sex with men. Sex Addict Compulsivity. 2014; 21:240–261.
- 69. Bőthe B, Tóth-Király I, Á Zsila, Griffiths MD, Demetrovics Z, Orosz G. The development of the Problematic Pornography Consumption Scale (PPCS). J Sex Res. 2018; 55:395–406.
- 70. Cacioppo M, Gori A, Schimmenti A, Baiocco R, Laghi F, Caretti V. Development of a new screening tool for cyber pornography: psychometric properties of the Cyber Pornography Addiction Test (CYPAT). Clin Neuropsychiatr: J Treat Eval. 2018; 15:60–65.
- 71. Agustus P, Munivenkatappa M, Prasad P. Sexual functioning, beliefs about sexual functioning and quality of life of women with infertility problems. J Hum Reprod Sci. 2017; 10:213–220.
- 72. Avasthi A, Grover S, Jhirwal O. Dhat syndrome: a culture-bound sex related disorder in Indian subcontinent. In: Sexually Transmitted Infections. 2nd ed. New Delhi, India: Elsevier; 2012.
- 73. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington: American Psychiatric Publishing; 2013.
- 74. Brock GB, Lue TF. Drug-induced male sexual dysfunction. An update. Drug Saf. 1993; 8:414–426.
- 75. de Boer MK, Castelein S, Wiersma D, Schoevers RA, Knegtering H. A systematic review of instruments to measure sexual functioning in patients using antipsychotics. J Sex Res. 2014; 51:383–389.
- 76. Symonds T, Abraham L, Bushmakin AG, Williams K, Martin M, Cappelleri JC. Sexual function questionnaire: further refinement and validation. J Sex Med. 2012; 9:2609–2616.
- 77. Levine SB. The nature of sexual desire: a clinician’s perspective. Arch Sex Behav. 2003; 32:279–285.
- 78. Cappelleri JC, Rosen RC. The Sexual Health Inventory for Men (SHIM): a 5-year review of research and clinical experience. Int J Impot Res. 2005; 17:307–319.
- 79. Meston C, Seal B, Hamilton L. Problems with arousal and orgasm in women. In: Handbook of Sexual and Gender Identity Disorders. Hoboken, NJ, USA: John Wiley & Sons, Inc.; 2008.
- 80. Serefoglu EC, McMahon CG, Waldinger MD An evidence-based unified definition of lifelong and acquired premature ejaculation: report of the second international society for sexual medicine ad hoc committee for the definition of premature ejaculation. Sex Med. 2014; 2:41–59.
- 81. Byers ES. Relationship satisfaction and sexual satisfaction: a longitudinal study of individuals in long-term relationships. J Sex Res. 2005; 42:113–118.
- 82. Gardner DG, Cummings LL, Dunham RB, Pierce JL. Single-item versus multiple-item measurement scales: an empirical comparison. Educ Psychol Meas. 1998; 58:898–915.
- 83. Zimmer K, Ellermeier W. Psychometric properties of four measures of noise sensitivity: a comparison. J Environ Psychol. 1999; 19:295–302.
- 84. Byers ES, MacNeil S. Further validation of the interpersonal exchange model of sexual satisfaction. J Sex Marital Ther. 2006; 32:53–69.
- 85. Flynn KE, Lin L, Bruner DW Sexual satisfaction and the importance of sexual health to quality of life throughout the life course of US adults. J Sex Med. 2016; 13:1642–1650.
- 86. Khazaei M, Rostami R, Zaryabi A. The relationship between sexual dysfunctions and marital satisfaction in Iranian married students. Procedia Soc Behav Sci. 2011; 30:783–785.
- 87. Carey MP, Spector IP, Lantinga LJ, Krauss DJ. Reliability of the Dyadic Adjustment Scale. Psychol Assess. 1993; 5:238–240.
- 88. Maroufizadeh S, Almasi-Hashiani A, Amini P, Sepidarkish M, Omani-Samani R. The Quality of Marriage Index (QMI): a validation study in infertile patients. BMC Res Notes. 2019;12:507.
- 89. Graham JM, Diebels KJ, Barnow ZB. The reliability of relationship satisfaction: a reliability generalization meta-analysis. J Fam Psychol. 2011; 25:39–48.
- 90. Rust J, Bennun I, Crowe M, Golombok S. The GRIMS: a psychometric instrument for the assessment of marital discord. J Fam Ther. 1990; 12:45–57.
- 91. Traeen B, Nilson TS. Use of pornography in traditional media and on the internet in Norway. J Sex Res. 2006; 43:245–254.
- 92. McKenna KYA, Green AS, Smith PK. Demarginalizing the sexual self. J Sex Res. 2001; 38:302–311.
- 93. de Alarcón R, de la Iglesia JI, Casado NM, Montejo AL. Online porn addiction: what we know and what we don’t—a systematic review. J Clin Med. 2019;8(1):91. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6352245/
- 94. Griffiths M. A ‘components’ model of addiction within a biopsychosocial framework. J Subst Use. 2005; 10:191–197.