INTRODUCTION
Airway compromise is the third leading cause of preventable battlefield deaths. Proficiency in securing airways using various methods is thus crucial for both hospital and prehospital personnel. However, placing a definitive airway device (such as an endotracheal tube [ETT]) is particularly challenging in prehospital scenarios, requiring extensive training and practice. Combat medics, often the first responders, may not have the skills or equipment for direct laryngoscopy, as one study evaluating the contents of combat medics’ aid bags revealed that none contained equipment needed for an advanced airway. Therefore, reliance on alternative methods, such as placement of supraglottic airway (SGA) devices, is often the focus of medics’ training and equipment.
The Tactical Combat Casualty Care Guidelines, key in directing field medical practices, have shifted preferences among SGA devices over time, with the i-gel gaining and then losing specific recommendations. Despite their possible utility, techniques like blind digital intubation (establishing a definitive airway by palpation alone without direct or fiberoptic laryngoscopy) and blind airway exchange via passing an introducer device through an SGA device remain controversial because of variable success rates and are generally discouraged. Although promising in early studies, these techniques have shown inconsistent results in later evaluations.
However, the Aintree intubation catheter (AIC) has been used effectively for exchanging airway devices through supraglottic devices, particularly in conjunction with the i-gel SGA device. It has been shown to reduce the risk of mechanical injury to the airway and provides a rapid and easy method for conversion to a cuffed tracheal tube. Therefore, our study seeks to determine if, despite variable success with blind intubation using other devices and methods, the AIC would be an effective adjunct for military medical personnel to conduct blind intubations by introducing it through an i-gel device.
Blind intubations, often conducted with an SGA device in place, involve using an introducer like the AIC or the gum elastic bougie (GEB). While the SGA device is in place, the user attempts to insert the introducer through the SGA device and into the trachea blindly, then removes the SGA device, and tries to pass an ETT over the introducer into the trachea. Our study aims to compare the AIC and GEB in blind airway exchanges through an i-gel SGA device in simulated prehospital environments, comparing the success rates and time efficiency of these exchanges.
We chose the i-gel because of its history of successful use in prehospital settings, its relative ease of placement without the need for cuff inflation, and its current status as the SGA device of choice listed in Tactical Combat Casualty Care guidelines. This study’s setting replicates prehospital conditions, acknowledging the limitations in generalizability because of the specific participant group and cadaver models used.
METHODS
Study Design
This randomized, crossover cadaver study was approved by the Carl R. Darnall Army Medical Center Human Research Protections Office as an Institutional Review Board (IRB)–exempt study. We designed it to compare the AIC and the GEB for airway exchange using the i-gel SGA device in a simulated prehospital setting. The primary outcome measured was the success rate of exchange tube intubation (ETI) between two airway introducer devices, the AIC and the GEB. The secondary outcome was time to successful airway exchange between the two devices.
We conducted this study in a controlled environment, using nonembalmed cadaver models to closely replicate real-life tissue characteristics and airway scenarios.
Study Population
We included a convenience sample of Army active duty volunteers completing training at the installation Medical Simulations Training Center (MSTC). Forty-eight participants enrolled and were randomly designated to start with either the AIC or GEB. The participants performed ETIs in a random order generated using a sequence generator (http://www.random.org). Study participants were Army combat medics (68W), physician assistant (PA) students, certified PAs, emergency medicine (EM) residents, and attending EM physicians. Although it is unlikely that combat medics would perform airway exchange in a prehospital setting, since these medics were in the process of performing airway training and since this was a convenience sample, we included them as participants.
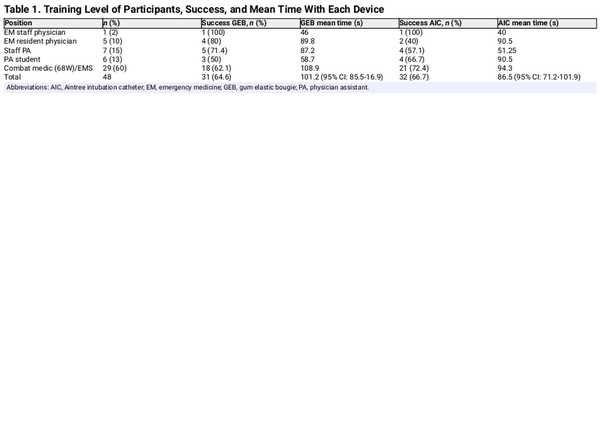
All participants completed a brief verbal questionnaire regarding demographic information (age and sex), professional medical title, and overall medical experience (Table 1). Before starting, instructors gave 10-minute lectures describing the different introducers and step-by-step instructions.
Data Collection
Investigators used the Cormack Lehane criteria to identify cadavers having grade I or II airways to limit confounding of success by cadavers having difficult airways. The authors originally planned to use 6 cadavers, but only 2 met this criterion. We did not collect identifying or demographic data on the cadaver models.
Investigators gave participants a brief demonstration of the required steps of the airway exchange to familiarize them with the necessary task. No practice iterations were allowed. The cadaver model started with an i-gel SGA device in place. We randomized participants to start with the AIC or GEB to eliminate recall bias. We placed all necessary materials to complete the task at the bedside for the participant.
On the command “go,” a research team member started a timer, and the participant took the introducer they were randomized to begin with and attempted to blindly pass the device through the opening of the i-gel into the trachea. Once they felt confident that they were in the trachea, they removed the i-gel and then threaded a standard 7.5-mm ETT over the device into the trachea. They then advanced the ETT to 21 cm at the teeth, removed the exchange device, and inflated the cuff. When the participants signaled that they had completed the airway exchange, researchers stopped their time and recorded the results. The research study team members then confirmed the placement of the ETT using direct laryngoscopy. If the research team member confirmed proper placement, the participant would use the same cadaver to transition to the other airway device. Following unsuccessful exchanges, the research team reset the cadaver, and the participant had 2 additional attempts. Once the participant completed an exchange or made 3 attempts, the research team reset the cadaver, and the participant completed the same process with the other introducer.
Data Analysis
We conducted all statistical analyses using the JMP Pro 16 software package. We could not find prior studies comparing these two devices, so we estimated a 50% difference in success rates between the two devices. Based on the assumed 50% discordance between devices, an alpha of 0.5, powered to 80%, we estimated that we would need 34 participants to detect a statistically significant difference.
We analyzed the categorical primary outcome, success rate with each device, using chi-square testing. We used the t-test to analyze the parametric secondary outcome of time to successful intubation.
RESULTS
Data collection occurred in two different iterations occurring between June and August 2022. The 48 participants included 29 Army combat medics, 6 PA students, 7 EM PA staff and trainees, and 6 EM attending and resident physicians (Table 1). The participants completed a total of 201 airway exchange attempts. The 201 attempts include 105 with the GEB and 96 with the AIC.
There was no significant difference in success rates between the 2 devices. Of the 201 attempts, 63 were successful ETIs, 31 with the GEB and 32 with the AIC. Participants demonstrated an overall 30% success rate with the GEB and 33% with the AIC, P = .56 (Table 1).
The authors recorded the secondary outcome measure of time to completion of a successful ETI in seconds from the command of “go” to the point when the participant indicated task completion. There was also no significant difference between the mean times for successful ETI with the devices. The overall mean time to success with the GEB was 101.2 seconds (95% CI, 85.5 to 116.9) and 86.5 seconds (95% CI, 71.2 to 101.9) with the AIC, P = .18 (Table 1, Figure 1).
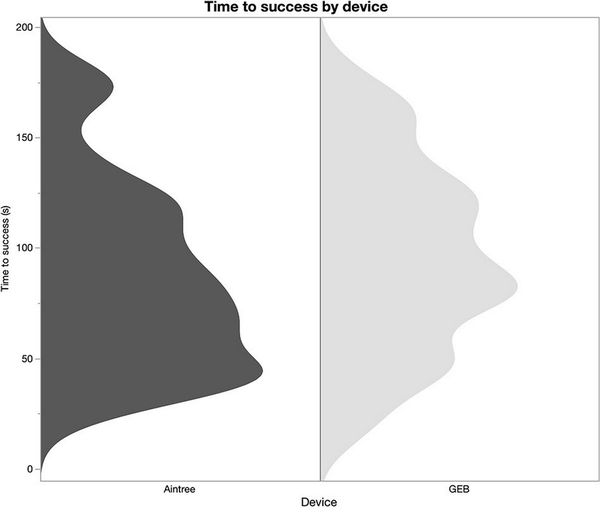
Figure 1
Histogram comparing time to success by device (in seconds).
Despite the absence of statistical significance, the AIC appeared to have performed slightly better than the GEB in both the primary and secondary outcomes. Primary outcome statistics revealed the AIC success rate to be 33% compared to the GEB of 30%. Additionally, when analyzing the success rate of the participants (n = 48) instead of the total number of attempts, the AIC performed slightly better than the GEB, 66.7% versus 64.6%, respectively (Table 1).
Separately, to determine if there was a difference in success based on the training level, we reported success rates between the two ETT introducers for the five subgroups: Attending EM physicians, resident EM physicians, PAs, PA students, and Army combat medics and emergency medical services technicians (EMS). The single attending physician was successful in both the GEB and AIC. Of the resident physicians (n = 5), 4 were successful in the GEB and 2 were successful in the AIC (80% and 40%, respectively). Of the PA group (n = 7), 5 were successful with the GEB and 4 were successful with the AIC (71% and 57%, respectively). Of the PA students (n = 6), 3 were successful with the GEB and 4 were successful with the AIC (50% and 66%, respectively). Finally, of the Army combat medics and EMS (n = 29), 18 were successful in the GEB and 21 were successful in the AIC (62% and 72%, respectively) (Table 1).
DISCUSSION
This study describes the performance between 2 ETT introducers when utilized as part of a blind airway exchange from an in-place i-gel. Typically, the AIC is used with fiberoptic bronchoscopy, and the GEB is used as a sole device to guide into the vocal cords, over which the ETT can later be rapidly placed. This study did not put the participants in either of those scenarios; instead, we expected them to attempt a blind insertion into the vocal cords through a correctly placed i-gel. The primary outcome measured the success rate, and the secondary measured the time to completion of the successful attempt. Although there is no statistical difference when comparing the success rate and time to completion between the 2 ETT introducers, the AIC appeared to have performed slightly better than the GEB overall.
When measuring total successful attempts, the AIC success rate is 30% compared to the GEB of 29%. Additionally, when analyzing the success rate of the participants (n = 48) instead of the total number of attempts, the AIC performed slightly better than the GEB, 66% versus 64%, respectively. Although the AIC was novel for all participants, it showed a slightly higher chance of success. The fact that the AIC performed similar to the GEB, which was already familiar to all participants, surprised the authors. The authors believe that this finding may be due to the lack of a coude tip in the AIC, which may have allowed the AIC to pass more easily into the vocal cords after emerging from the other end of the i-gel. Conversely, the coude tip of the GEB may have added difficulty because of its more anterior angle as it emerged from the i-gel. As the i-gel’s intended purpose is to allow passage of oxygen into the vocal cords and trachea, the lack of a curved tip may have allowed a better trajectory for the AIC as it emerged.
The secondary outcome measured the mean time to completion of successful attempts. Although not statistically significant, the findings showed participants completing the successful attempts faster with the AIC than with the GEB. As stated in the previous paragraph, this finding may be due to the i-gel mold and its intended purpose and the lack of a coude tip on the AIC. However, it took participants a significant amount of time to exchange the i-gel for an ETT with both devices, which practitioners should consider when attempting an airway exchange on a critically ill patient.
The difference in size between the two introducers did not appear to affect the findings. The AIC has a slightly larger external diameter of 19 French (6.5 mm) versus the GEB’s 15 French (5 mm). The AIC’s larger diameter did not affect its performance compared to the GEB in primary and secondary outcomes.
The results of our study conflict with the findings of similar previous studies. One prior study with similar designs, including cadaveric tissue, AIC use, and airway exchange via blind intubations, found the success rate for the AIC to be 56.8% via the i-gel. Our study underperformed with a success rate of 33%, possibly because of having only utilized two cadavers versus their six. Notably, however, their participants included a higher proportion of emergency physicians and residents, which may also have impacted their success rates.
Additionally, a manikin study comparing the two devices found that the GEB performed better than the AIC in blind intubations: 64% versus 47%, respectively. This study also used the i-gel device. However, it is unclear how the use of manikins versus cadaveric tissue may have impacted these results.
Limitations
Although the number of enrolled participants exceeded the recommended sample size analysis of 34, our study appeared to have found no statistical significance between the two ETT introducers. A larger sample size may have led to a finding of statistical significance.
Additionally, our study had significantly disproportionate subgroup participants. For example, of the 48 participants, 1 was an attending physician, 5 were resident physicians, 7 were certified PAs, 6 were PA students, and 29 were Army combat medics or EMS personnel. The combat medics comprised more than half of the sample. Previous studies appeared to have had appropriate representation and statistically significant findings using single subgroup enrollments, such as a cited study that included only anesthesiologists. Furthermore, despite making up more than half of the participants, ETT insertion is beyond the scope of practice of most combat medics who are note paramedic certified.
As a single-center study, the investigators were limited to the availability and suitability of cadavers. The investigators used the Medical Simulation Training Center’s (MSTC) building and cadavers to collect data. The authors were limited to choosing from the cadavers obtained by the MSTC, which were also used for a separate training event during data collection. Of the limited selection, only two met the Cormack Lehane grading system of I or II.
Cadaveric tissue does not respond the same way as live tissue. Repeated attempts on the same cadaver may have caused distortions of the airway tract, leading to false or accessory tracts. Additionally, given that participants performed blind airway exchanges, the risk of creating and placing the ETT introducer into a false tract was likely higher than if conducted using direct or video laryngoscopy or fiberoptic bronchoscopic visualization. The use of more than two cadavers may have also decreased the incidence of creating false tracts.
Our team did not implement a Likert survey, which would have allowed participants to provide feedback on the devices. Such a survey would have provided valuable findings, given the novelty of the AIC compared to the more familiar GEB.
Finally, our study only utilized cadavers with Cormack Lehane grade I or II airways. While we assumed that cadavers with less difficult airways would reduce the confounding of results, this choice further limits the generalizability of our results to those with more challenging airways.
CONCLUSION
This study attempted to demonstrate statistical significance in success rate and time to completion of successful iterations of airway exchanges between two ETT introducers via an in-place i-gel while utilizing cadavers. Following analysis, neither device performed significantly better in success rate or time to completion. Although the AIC performed slightly better overall, there is insufficient statistical significance to argue its superiority over the GEB.
However, our study clearly indicates that blind SGA device to ETT exchanges using the AIC or GEB should not be recommended for routine practice, especially in prehospital settings. The low success rates and the potential for airway tract damage in repeated attempts underscore the need for alternative airway management strategies or significant training improvements.
REFERENCES
- 1. Bellamy RF. The causes of death in conventional land warfare: implications for combat casualty care research. Mil Med. 1984;149(2):55–62.doi: 10.1093/milmed/149.2.55
- 2. Maughon JS. An inquiry into the nature of wounds resulting in killed in action in Vietnam. Mil Med. 1970;135(1):8–13.doi: 10.1093/milmed/135.1.8
- 3. Holcomb JB, McMullin NR, Pearse L, et al. Causes of death in U.S. Special Operations Forces in the global war on terrorism: 2001–2004. Ann Surg. 2007;245(6):986–91.doi: 10.1097/01.sla.0000259433.03754.98
- 4. Kelly JF, Ritenour AE, McLaughlin DF, et al. Injury severity and causes of death from operation Iraqi freedom and operation enduring freedom: 2003–2004 versus 2006. J Trauma. 2008;64(2):S21–7.
- 5. Schauer SG, Naylor JF, Uhaa N, April MD, De Lorenzo RA. An inventory of the combat medics. Aid Bag J Spec Oper Med. 2020;20(1):61.doi: 10.55460/FUHO-CU87
- 6. Anonymous A. Tactical Combat Casualty Care (TCCC) Guidelines for Medical Personnel 15 December 2021. J Spec Oper Med. 2022;22(1):11.doi: 10.55460/ETZI-SI9T
- 7. Chadd GD, Ackers JWL, Bailey PM. Difficult intubation aided by the laryngeal mask airway. Anaesthesia. 1989;44(12):1015.doi: 10.1111/j.1365-2044.1989.tb09244.x
- 8. Allison A, McCrory J. Tracheal placement of a gum elastic bougie using the laryngeal mask airway. Anaesthesia. 1990;45(5):419–20.doi: 10.1111/j.1365-2044.1990.tb14809.x
- 9. Murdoch JAC. Emergency tracheal intubation using a gum elastic bougie through a laryngeal mask airway. Anaesthesia. 2005;60(6):626–7.doi: 10.1111/j.1365-2044.2005.04248.x
- 10. Gabbott DA, Sasada MP. Tracheal intubation through the laryngeal mask using a gum elastic bougie in the presence of cricoid pressure and manual in line stabilisation of the neck. Anaesthesia. 1996;51(4):389–90.doi: 10.1111/j.1365-2044.1996.tb07754.x
- 11. Ahmed AB, Nathanson MH, Gajraj NM. Tracheal intubation through the laryngeal mask airway using a gum elastic bougie: the effect of head position. J Clin Anesth. 2001;13(6):427–9.doi: 10.1016/S0952-8180(01)00295-1
- 12. Lefevre RJ, Jelly CA, Schmelz C, et al. Comparison of i-gel® and LMA® Supreme™ for facilitating fiberoptic endotracheal intubation: a prospective randomized trial. AANA J. 2024;92(3):197–205.
- 13. Ueki R, Komasawa N, Nishimoto K, et al. Utility of the Aintree Intubation Catheter in fiberoptic tracheal intubation through the three types of intubating supraglottic airways: a manikin simulation study. J Anesth. 2014;28(3):363–7.doi: 10.1007/s00540-013-1724-3
- 14. Olesnicky BL, Rehak A, Bestic WB, Brock JT, Watterson L. A cadaver study comparing three fibreoptic‐assisted techniques for converting a supraglottic airway to a cuffed tracheal tube. Anaesthesia. 2017;72(2):223–9.doi: 10.1111/anae.13733
- 15. Chae YJ, Lee H, Jun B, Yi IK. Conversion of I-gel to definitive airway in a cervical immobilized manikin: Aintree intubation catheter vs long endotracheal tube. BMC Anesthesiol. 2020;20(1):152.doi: 10.1186/s12871-020-01069-9
- 16. Benger JR, Lazaroo MJ, Clout M, et al. Randomized trial of the i-gel supraglottic airway device versus tracheal intubation during out of hospital cardiac arrest (AIRWAYS-2): patient outcomes at three and six months. Resuscitation. 2020;157:74–82.doi: 10.1016/j.resuscitation.2020.09.026
- 17. Lopez NT, McCoy SK, Carroll C, Jones E, Miller JA. Non-conventional utilization of the aintree intubating catheter to facilitate exchange between three supraglottic airways and an endotracheal tube: a cadaveric trial. Mil Med. 2019;184(1–2):e222–8.doi: 10.1093/milmed/usy144
- 18. Michalek P, Donaldson W, Graham C, Jd H. A comparison of the I-gel supraglottic airway as a conduit for tracheal intubation with the intubating laryngeal mask airway: a manikin study. Resuscitation. 2010;81(1):74–7.doi: 10.1016/j.resuscitation.2009.10.009