An estimated one third of hepatitis C virus (HCV)-infected individuals in the United States spend at least part of the year in a correctional facility []. United States jails detain those awaiting trial or serving sentences of maximum 1-year duration. Among individuals tested in the New York City (NYC) jails during 2013–2014 using a risk factor-based and 1945–1965 birth cohort-based screening strategy, 21% were HCV antibody-positive []. Achieving national goals for HCV elimination [] will require scaling up treatment for people who are incarcerated, including those in jail. United States guidelines recommend treating HCV-infected individuals who are incarcerated with direct-acting antiviral (DAA) therapy and providing linkage to community healthcare upon discharge from correctional settings []. Although retaining people who inject drugs (PWID) in care to confirm sustained virologic response at 12 weeks (SVR12) can be challenging [], real-world data has shown effectiveness of DAA therapy among PWID in a variety of settings and care models [, ].
Challenges to HCV treatment in jails include short and unpredictable lengths of stay (median 19 days for admissions to NYC jails during 2018) [] and low rates of linkage to community care after discharge (range, 9%–31%) [, ]. Treatment in prisons has scaled up in a number of states, but gaps remain (range, 0.1%–28.4% of HCV-infected persons treated per year) []. With an estimated 50% of individuals who recently injected drugs infected with HCV globally [], modeling predicts that scaling up DAA treatment and opioid agonist therapy (OAT) among incarcerated PWID with opioid use disorder can reduce HCV incidence and prevalence []. Implementing DAA therapy for HCV has been successful with high cure rates in prison settings [], but little has been published from jail settings. Treatment with DAA therapy in NYC jails is feasible as reported in a prior study from our system [], but this study did not report SVR12 data and surveillance for reinfection events, due to lack of longitudinal follow-up.
Patients treated for HCV in NYC jails either started treatment in the community or while in jail. We hypothesized that the latter group was less likely to have established HCV care in the community, and this may influence their treatment outcomes. Those who started treatment in the community were all engaged in healthcare services that included the ability to assess HCV and prescribe medications, but this may not be true for those who started treatment in jail. The latter group may have more difficulty completing treatment or getting an SVR12 laboratory test result checked if they were discharged from jail before those milestones. To test this hypothesis, we compared outcomes between those in our cohort who started treatment in the community versus in jail. This study aims to characterize the outcomes of HCV-infected individuals treated with DAA therapy in the NYC jail system. We report data on frequency of SVR12 confirmation, the proportion who achieve SVR12, and the incidence of recurrent viremia events.
METHODS
Study Population
In calendar year 2017, NYC jails had an average daily population of ~9150 with >55 000 admissions (internal data, Correctional Health Services). We performed a retrospective observational cohort study including all patients in NYC jails who were treated with DAA therapy for HCV while in jail starting from January 15, 2014 to October 2, 2017, regardless of whether they were released from jail. The last patient completed treatment on December 24, 2017. For the incarceration during which they were treated, all patients in our cohort were released from jail by November 8, 2018. Some patients initiated DAA treatment in jail, whereas others initiated treatment in the community and then were incarcerated. Some patients finished treatment in jail, whereas others were released from jail while still on treatment.
Treatment
Healthcare in the jails is provided by Correctional Health Services (CHS), a division of NYC Health + Hospitals, the city’s public healthcare system. Healthcare delivery, including HCV treatment, is funded directly by the city. Patients with HCV infection were referred to jail-based infectious diseases physicians to be evaluated for treatment. Treatment was started in jail if estimated length of stay was enough to complete treatment in jail or if there was clinical urgency, such as advanced liver disease, regardless of length of stay. The DAA regimen selection was based on the prescriber’s clinical assessment along with consideration of current CHS formulary agents and clinical practice guidelines []. In addition, all newly admitted patients were asked whether they were on HCV treatment started in the community. Treatment regimens started in the community were verified with the community prescriber and continued. Most of these patients were continued on HCV treatment within 1–2 days of jail admission. When there was an inadvertent delay in continuing therapy, we extended the regimen duration to make up for the treatment gap. Patients who were released to the community mid-treatment were provided a 7-day supply of DAA medications at the point of jail discharge, and efforts were made to link them to care to complete treatment.
Outcomes
We compared outcomes in 2 groups: patients who started treatment in the community and those who started in jail. Our primary outcome was SVR12, defined as an undetectable HCV ribonucleic acid (RNA) level according to the reference range set by the test manufacturer, checked ≥64 days after the projected end date of the treatment course. The 64-day time point was used by another recent real-world treatment outcomes study to allow for a window around usual clinical care []. Additional outcomes were (1) proportion of our cohort with SVR12 virologic data available and (2) incidence of recurrent viremia events.
A recurrent viremia event was defined as a detectable HCV RNA level among those who achieved SVR12 and had a subsequent HCV RNA level checked. All who achieved SVR12 and had a subsequent HCV viral load test contributed to follow-up time. For those with recurrent viremia, we used the midpoint between the dates of the first positive viral load after SVR12 was achieved and the preceding undetectable viral load to calculate follow-up time, an approach used by others []. Follow-up time had to be estimated because our cohort did not have systematic regular assessments of HCV viral load after treatment. We do not know when the recurrent viremia occurred between a negative viral load followed by a positive one.
Data Collection
Cohort characteristics were gathered from the CHS electronic health record (EHR) through structured data reports and chart review, and the CHS HCV treatment tracking database. We extracted the following variables from the EHR: date of birth, sex, race/ethnicity, human immunodeficiency virus (HIV) diagnosis, advanced fibrosis or cirrhosis status, diagnosis of serious mental illness (SMI), and homelessness status and data on probable alcohol and opioid use disorder. Human immunodeficiency virus infection status was defined by either self-report at intake or positive serology. Advanced fibrosis or cirrhosis was defined as either a FIB-4 score >3.25 [] or FibroSure (LabCorp, Burlington, NC) fibrosis stage of ≥F3.
Patients were designated by the mental health service to have SMI according to CHS policy, which changed during the study period but comprised mainly patients diagnosed with psychotic disorders, bipolar disorder, depressive disorders, and, in the last year of the study period, posttraumatic stress disorder. History of homelessness was captured by patient self-report, although this status was not routinely ascertained during this period. Probable alcohol use disorder was defined as (1) patient self-report with or without use of chlordiazepoxide taper to prevent withdrawal on admission or (2) the presence of an International Statistical Classification of Diseases and Related Health Problems (ICD) 9/10 diagnosis code []. Probable opioid use disorder was defined based on review of available data including positive self-report, positive urine toxicology screening on medical intake, any methadone or buprenorphine prescription, or presence of an ICD 9/10 diagnosis code. We defined OAT as receiving methadone (≥20 mg) or buprenorphine (≥2 mg) 3 or fewer days before discharge, a definition used in the literature []. Jail lengths of stay were calculated from admission, and discharge dates were extracted from the EHR. We obtained HCV treatment regimen information from the CHS treatment tracking database.
Aggregate virologic data on whether patients had SVR12 results and subsequent recurrent viremia were based on HCV laboratory surveillance data electronically reported to the NYC Department of Health and Mental Hygiene (DOHMH). Mandated by law, the DOHMH receives positive HCV antibody, positive and negative HCV viral load, and genotype results processed in NYC laboratory facilities, including tests done on individuals incarcerated in the NYC jail system. Test results from May 2, 2014 (earliest planned treatment end date) to December 31, 2018 were included in this analysis.
Statistical Analysis
We used descriptive statistics and χ 2 and Mann-Whitney U tests to characterize and compare jail-initiated and community-initiated groups. The SVR12 frequency was expressed as a percentage of those who had an undetectable HCV viral load among those with SVR12 virologic data available. We performed an equivalent analysis for our secondary outcomes of recurrent viremia events and the proportion of our entire cohort who had SVR12 virologic data available. We calculated risk ratios of achieving SVR12 and having SVR12 virologic data available using log-binomial regression. Multivariable models were built to test for independent association of patient and treatment characteristics with these 2 outcomes. Significance was defined as a 2-sided P < .05. All statistical analysis was carried out using SAS software version 9.4 (SAS Institute, Inc., Cary, NC) and SPSS software version 24 (IBM, Somers, NY).
Study Oversight
This study protocol was reviewed and approved by a third-party institutional review board (BRANY, Lake Success, NY).
RESULTS
Patient Characteristics
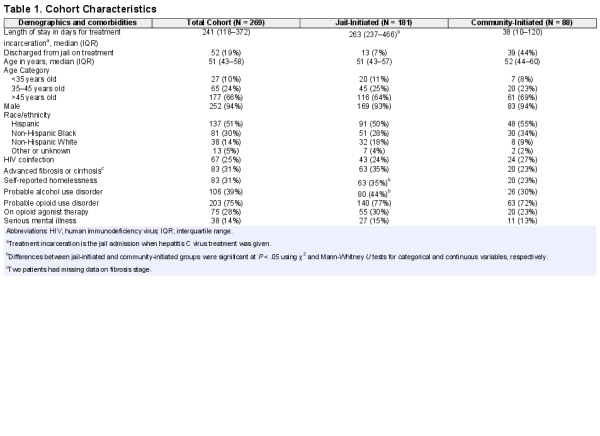
There were 269 patients in our cohort who were treated with DAA therapy while in jail. Treatment was started in jail for 181 patients (67%) and continued for 88 patients (33%) who initiated it in the community. Of the 269 patients, 214 (80%) completed treatment in jail, 52 (19%) were released to the community on treatment, and 3 (1%) discontinued treatment while in jail (Figure 1). Of the patients who did not complete treatment in jail, the median duration of treatment completed on day of discharge was 57 days (interquartile range [IQR], 35–75), including treatment before incarceration. There were 254 (94%) patients who received 84-day treatment regimens, 13 (5%) who received 168-day regimens, and 2 (1%) who received 56-day regimens. Most had genotype 1 (80%) or 3 (9%) infection. The cohort was 94% male with a median age of 51 years (IQR, 43–58) (Table 1). There were 67 (25%) patients coinfected with HIV, 83 (31%) with advanced fibrosis or cirrhosis, 83 (31%) with a history of homelessness before incarceration, and 38 (14%) with SMI. Patients who started on treatment in jail had a significantly higher prevalence of self-reported homelessness (35% vs 23%, P < .05) and alcohol use disorder (44% vs 30%, P < .05), compared to the patients started on treatment in the community (Table 1).
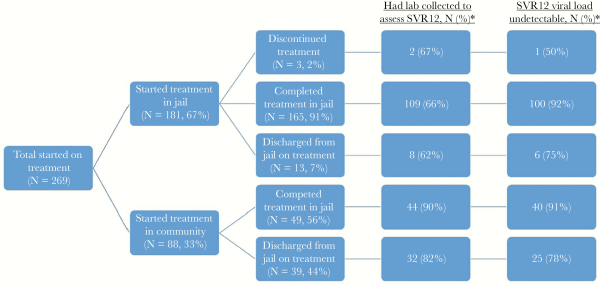
Figure 1
Treatment cascade of care. *, Percentages are based on previous step as denominator. lab, laboratory SVR12, sustained virologic response at 12 weeks.
Sustained Virologic Response at 12 Weeks Outcomes
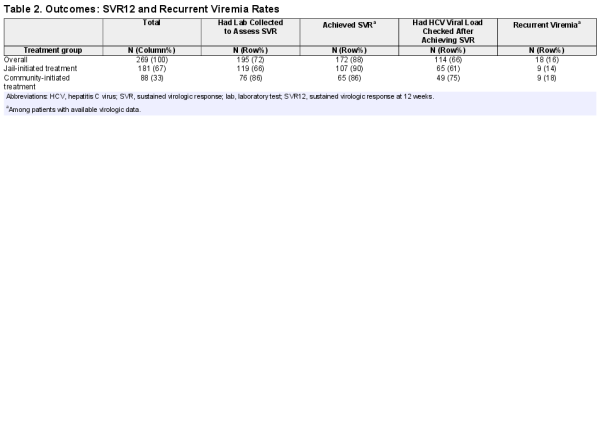
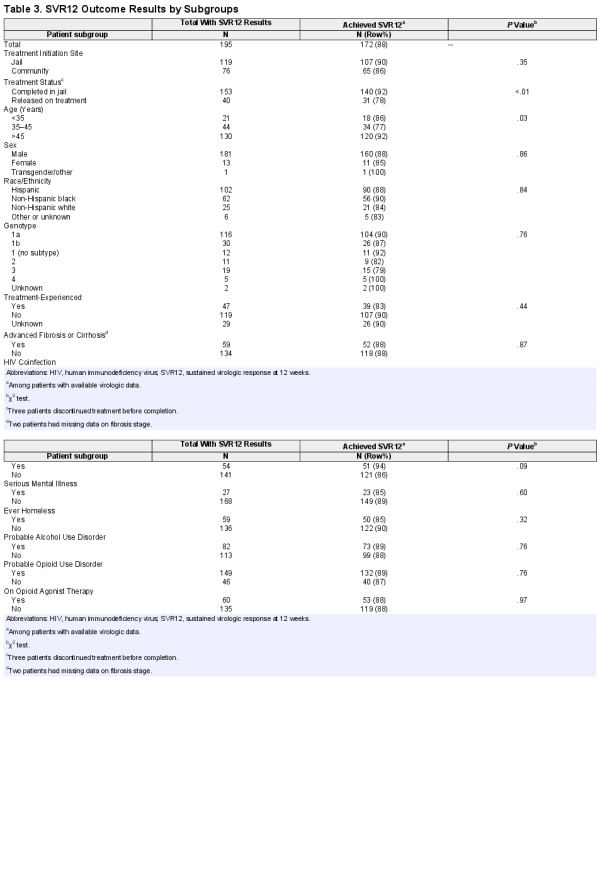
Of the 269 patients in our cohort, 195 (72%) had SVR12 data, 172 (88%) of which achieved SVR12 (Table 3). Treatment completion in jail was significantly associated with achieving SVR12, relative to being released on treatment (92% vs 78%, χ 2P < .01; unadjusted risk ratio [RR], 2.85; 95% confidence interval [CI], 1.29–6.29). When adjusted for age and race/ethnicity, the association remained significant (adjusted RR, 2.93; 95% CI, 1.35–6.34). Treatment initiation site was not associated with achieving SVR12. Age category was significantly associated with achieving SVR12 in bivariate analysis, but there was no trend by age group. No other factors were associated with achieving SVR12.
Recurrent Viremia Events
Of the 172 patients who achieved SVR12, 114 (66%) had at least 1 subsequent viral load, and 18 (16%) had recurrent viremia (Table 2). The 114 patients contributed 170 person-years (PY) of follow-up (median, 500 days; IQR, 235–814), resulting in a recurrent viremia rate of 10.6 cases per 100 PY.
Comparison Between Those With and Without Sustained Virologic Response at 12 Weeks Virologic Outcome Data
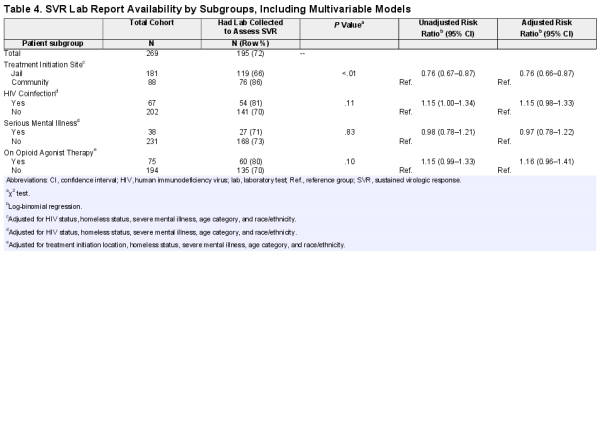
There were 74 (28%) patients in our cohort who never had a laboratory test collected to assess SVR12. Of these patients, 28 (38%) were in jail at the SVR12 time point. Of the analyzed variables, those who initiated treatment in jail were less likely to have an SVR12 laboratory test result checked than those who initiated treatment in the community (66% vs 86%, P < .01; unadjusted RR, 0.76; 95% CI, 0.67–0.87) (Table 4). After adjusting for age, race/ethnicity, HIV status, history of homelessness, and severe mental illness, the association remained significant (adjusted RR, 0.76; 95% CI, 0.66–0.87).
DISCUSSION
This study reports outcomes of the largest real-world cohort of HCV treatment with DAA therapy in a US jail system. Our results demonstrate that treatment is feasible and effective, with a cure rate (88%) among those with virologic data that approaches those in contemporary real-world studies (94%–96%) []. Our cohort had a high prevalence of self-reported homelessness, substance use, and mental illness, all of which have been cited as barriers to HCV care during the DAA treatment era []. Jail-based treatment initiation is an effective strategy to reach these marginalized populations. Our cohort also had a high percentage of HIV-HCV-coinfected patients (25%) who are at risk for accelerated liver fibrosis progression []. Consistent with treatment guidelines during the study time frame [], there was some effort to prioritize their HCV treatment. Since then, our HCV treatment cohort has had a lower prevalence of HIV coinfection (8%; internal data), reflecting efforts to treat broadly regardless of medical comorbidities. Our data also highlight ongoing challenges related to unpredictable lengths of stay in jail, loss to follow-up, and reinfection.
We analyzed the proportion of the cohort who had SVR12 virologic data available as an indicator of linkage to follow-up care after HCV treatment. In our cohort, those starting on treatment in jail were significantly less likely to have an SVR12 laboratory test done compared to those who started treatment in the community. This may be because patients who started treatment in the community have a healthcare provider to return to, whereas those starting treatment in jail may not have had pre-existing care in the community. In 2019, CHS launched Point of Transition and Reentry (PORT) clinics in the community designed to serve our patients recently discharged from jail. Patients without established care in the community can be seen for treatment completion and SVR12 laboratory tests. We also found that 28 of 74 (38%) individuals who did not have SVR12 status confirmed during our cohort follow-up were in jail at the SVR12 time point, indicating missed opportunities for follow-up while under CHS care. This finding has prompted us to implement additional measures to improve rates of checking SVR12 laboratory tests while incarcerated. For the most frequently incarcerated individuals, correctional settings may be the primary source of medical care outside of emergency services in the community. Efforts should be made to improve jail- and community-based follow-up for all treated patients to encourage confirmation of SVR12 status.
In our cohort, those discharged from jail on treatment were significantly less likely to achieve SVR12. This is consistent with the literature that suggests that release from custody during HCV therapy was associated with lower cure rates []. Reasons for this may include poor adherence to treatment upon return to the community or difficulty accessing medications due to delays in Medicaid reinstatement (Medicaid is suspended during incarceration) or insurance approvals for treatment continuation. These data argue for both completing treatment in jail when length of stay permits and improving community transitions of care to minimize treatment interruptions for those discharged mid-treatment. The median length of stay for the cohort that started treatment in jail was 263 days (IQR, 237–466), so if treatment started early during their stay, they had enough time to complete treatment in jail. Time available for treatment in jail was lost due to delays in completing the medical workup or estimating the jail length of stay. Therefore, shortening the time between jail admission and start of HCV treatment should be a focus of our quality improvement efforts.
It is encouraging that, among those with virologic data available, no other factors we analyzed were predictive of achieving SVR12, including mental illness, probable alcohol or opioid use disorder, or OAT status at discharge. Being on OAT was not associated with SVR12 in our analysis. Although OAT provision in correctional facilities improves morbidity and mortality and should be encouraged [], HCV treatment can be successful in people actively using drugs and not receiving OAT []. Being on OAT should not be a requirement for HCV treatment in people actively using drugs. Our study demonstrates DAA effectiveness and supports scaling up treatment in correctional settings where substance use disorders are highly prevalent. We observed a significantly higher frequency of achieving SVR12 in the older group (age >45 years) compared with the younger groups, which is consistent with other data on DAA treatment among people who use drugs []. However, there was no trend in the association between age group and achieving SVR12, so it is unclear what explains this finding. Lower SVR12 in the middle age group (age 35–45 years) could be due to a combination of early reinfection events, suboptimal treatment adherence, or other unmeasured confounders.
Our cohort demonstrated a higher rate of recurrent viremia (10.6 per 100 PY), likely representing reinfection, than recent data on reinfection rates among people actively using drugs after DAA treatment. The C-EDGE CO-STAR Part B study followed 199 individuals treated with elbasvir/grazoprevir with HCV viral loads every 6 months []. Reinfection rate over a 30-month follow-up period was 2.8 per 100 PY among patients who reported intravenous drug use during follow-up. Other studies have found similarly low rates of reinfection among PWID [], although a higher reinfection rate (10.2 per 100 PY; 95% CI, 3.74–22.2) was seen in one cohort of younger people actively injecting drugs []. Our high rates of reinfection likely reflect risky drug use behavior among our cohort, which had a high prevalence of opioid use disorder (76%), paired with a low proportion of individuals on OAT at discharge (28%). Strategies to minimize reinfection include treating injection networks [], increasing provision of OAT, and reducing harm through needle and syringe programs [, ]. Since September 2017, OAT provision in our jail health system has scaled up substantially. Future studies should examine whether this intervention was associated with lower rates of HCV reinfection.
Our study has limitations. Because we lack SVR12 virologic data on 28% of our cohort, our reported SVR12 could be biased toward those who are engaged in care. However, baseline factors of age, sex, race/ethnicity, presence of advanced fibrosis, severe mental illness, opioid use disorder, and history of homelessness were all not associated with having an SVR12 laboratory test checked. Therefore, there was no bias between the groups with and without SVR12 data based on key demographics and comorbidities. We did not have data on whether treatment was completed for individuals discharged from jail mid-treatment (N = 52), so we could not analyze whether treatment completion was associated with achieving SVR12. We did not capture virologic testing that was done outside of NYC. Some in our cohort may have had SVR12 laboratory tests checked in the NY state prison system or elsewhere outside of NYC. We also did not have mortality data. Some in our cohort may have died after treatment but before SVR12 could be checked. For those who did not achieve SVR12, we do not have HCV sequencing data to differentiate between relapse versus early reinfection. However, this would only bias our results toward a lower reported frequency of achieving SVR12. Although we do not know whether all the episodes of recurrent viremia signify reinfection, late relapse occurring after the SVR12 time point is rare with DAA therapy []. History of homelessness was not routinely asked of all admitted patients for most of the study period, so our data may underestimate prevalence. We did not investigate the association of reincarceration with our outcomes, but this should be analyzed with subsequent studies. Finally, given that jail-based correctional healthcare in the United States is funded by local budgets, our results may not be generalizable to other jail settings with different available resources.
Nevertheless, our data argue that HCV treatment can and should be initiated in US jails. Treatment should not be restricted to those with a defined jail sentence, because we demonstrated effectiveness in the vast majority of treated patients without making this a requirement. Fewer individuals would have received treatment if we focused on the sentenced population, which accounted for 14% of the jail census at the beginning of our DAA treatment program []. Simplified treatment algorithms [] along with expanded eligibility criteria for 8-week treatment regimens [] should be leveraged when clinically appropriate to allow more individuals to be treated in jail with shorter stays. Patient navigation strategies that have demonstrated early effectiveness in our setting [] should be further evaluated and scaled up to improve treatment outcomes when patients are discharged from jail.
CONCLUSIONS
In conclusion, we found that treatment of HCV with DAA therapy in a large urban jail was effective with high frequency of SVR12. Challenges related to scale up of treatment include avoiding interruptions upon return to the community, ensuring proper follow-up care, and minimizing reinfection. Future studies should evaluate strategies to improve these outcomes.
Acknowledgments
We thank Ruth Leibowitz and the Correctional Health Services (CHS) IT team for data retrieval from CHS electronic health records. We thank Monica Katyal and Janet Wiersema for critical review of the manuscript.
Author contributions. J. C., P. Y., and R. M. conceived of the project. J. C., J. S., F. K., L. H., and A. B. contributed to literature searches, study design, and data collection. J. C., J. S., F. K., A. B., and M. J. A. conducted data analysis. J. C., J. S., F. K., A. B., M. J. A., Z. R., A. W., P. Y., and R. M. conducted data interpretation. J. C., J. S., F. K., and A. B. drafted the manuscript. All authors critically reviewed and approved the final version.
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1. Varan AK, Mercer DW, Stein MS, Spaulding AC. Hepatitis C seroprevalence among prison inmates since 2001: still high but declining. Public Health Rep2014; 129:187–95.
- 2. Akiyama MJ, Kaba F, Rosner Z, et al Hepatitis C screening of the “Birth Cohort” (born 1945–1965) and younger inmates of New York City jails. Am J Public Health2016;106:1276–7.
- 3. National Academies of Sciences, Engineering, and Medicine. A National Strategy for the Elimination of Hepatitis B and C: Phase Two Report. Washington, DC: The National Academies Press; 2017.
- 4.
- 5. Morris L, Smirnov A, Kvassay A, et al Initial outcomes of integrated community-based hepatitis C treatment for people who inject drugs: findings from the Queensland Injectors’ Health Network. Int J Drug Policy2017; 47:216–20.
- 6. Eckhardt BJ, Scherer M, Winkelstein E, et al Hepatitis C treatment outcomes for people who inject drugs treated in an accessible care program located at a syringe service program. Open Forum Infect Dis2018; 5:ofy048.
- 7. Akiyama MJ, Norton BL, Arnsten JH, et al Intensive models of hepatitis C care for people who inject drugs receiving opioid agonist therapy: a randomized controlled trial. Ann Intern Med2019; 170:594–603.
- 8. NYC Health + Hospitals internal reports, March 2019.
- 9. Akiyama MJ, Columbus D, MacDonald R, et al Linkage to hepatitis C care after incarceration in jail: a prospective, single arm clinical trial. BMC Infect Dis2019; 19:703.
- 10. Hochstatter KR, Stockman LJ, Holzmacher R, et al The continuum of hepatitis C care for criminal justice involved adults in the DAA era: a retrospective cohort study demonstrating limited treatment uptake and inconsistent linkage to community-based care. Health Justice2017; 5:10.
- 11.
- 12. Grebely J, Hajarizadeh B, Dore GJ. Direct-acting antiviral agents for HCV infection affecting people who inject drugs. Nat Rev Gastroenterol Hepatol2017; 14:641–51.
- 13. Stone J, Martin NK, Hickman M, et al Modelling the impact of incarceration and prison-based hepatitis C virus (HCV) treatment on HCV transmission among people who inject drugs in Scotland. Addiction2017; 112:1302–14.
- 14. Sterling RK, Cherian R, Lewis S, et al Treatment of HCV in the department of corrections in the era of oral medications. J Correct Health Care2018; 24:127–36.
- 15. MacDonald R, Akiyama MJ, Kopolow A, et al Feasibility of treating hepatitis C in a transient jail population. Open Forum Infect Dis2017; 4:ofx142.
- 16.
- 17. Reddy KR, Lim JK, Kuo A, et al; HCV-TARGET Study Group. All-oral direct-acting antiviral therapy in HCV-advanced liver disease is effective in real-world practice: observations through HCV-TARGET database. Aliment Pharmacol Ther2017; 45:115–26.
- 18. Aitken CK, Agius PA, Higgs PG, et al The effects of needle-sharing and opioid substitution therapy on incidence of hepatitis C virus infection and reinfection in people who inject drugs. Epidemiol Infect2017; 145:796–801.
- 19. Sterling RK, Lissen E, Clumeck N, et al; APRICOT Clinical Investigators. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology2006; 43:1317–25.
- 20.
- 21. Marsden J, Stillwell G, Jones H, et al Does exposure to opioid substitution treatment in prison reduce the risk of death after release? A national prospective observational study in England. Addiction2017; 112:1408–18.
- 22. Pan CQ, Tiongson BC, Hu KQ, et al Real-world study on sofosbuvir-based therapies in Asian Americans with chronic hepatitis C. J Clin Gastroenterol2019; 53:147–54.
- 23. Haridy J, Wigg A, Muller K, et al; Adelaide Liver Group. Real-world outcomes of unrestricted direct-acting antiviral treatment for hepatitis C in Australia: The South Australian statewide experience. J Viral Hepat2018; 25:1287–97.
- 24. Trabut JB, Barrault C, Charlot H, et al Integrated care for the use of direct-acting antivirals in patients with chronic hepatitis C and substance use disorder. J Addict Med2018; 12:346–52.
- 25. Jain MK, Thamer M, Therapondos G, et al Has access to hepatitis C virus therapy changed for patients with mental health or substance use disorders in the direct-acting-antiviral period? Hepatology 2019; 69:51–63.
- 26. Madden A, Hopwood M, Neale J, Treloar C. Beyond interferon side effects: what residual barriers exist to DAA hepatitis C treatment for people who inject drugs?PLoS One2018; 13:e0207226.
- 27. Noska A, Belperio PS, Loomis TP, et al Engagement in the hepatitis C care cascade among homeless veterans, 2015. Public Health Rep2017; 132:136–9.
- 28. Kirk GD, Mehta SH, Astemborski J, et al HIV, age, and the severity of hepatitis C virus-related liver disease: a cohort study. Ann Intern Med2013; 158:658–66.
- 29. Aspinall EJ, Mitchell W, Schofield J, et al A matched comparison study of hepatitis C treatment outcomes in the prison and community setting, and an analysis of the impact of prison release or transfer during therapy. J Viral Hepat2016; 23:1009–16.
- 30. Malta M, Varatharajan T, Russell C, et al Opioid-related treatment, interventions, and outcomes among incarcerated persons: a systematic review. PLoS Med2019; 16:e1003002.
- 31. Norton BL, Fleming J, Bachhuber MA, et al High HCV cure rates for people who use drugs treated with direct acting antiviral therapy at an urban primary care clinic. Int J Drug Policy2017; 47:196–201.
- 32. Hajarizadeh B, Cunningham EB, Reid H, et al Direct-acting antiviral treatment for hepatitis C among people who use or inject drugs: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol2018; 3:754–67.
- 33. Grebely J, Litwin AH, Dalgard O, et al HCV reinfection and injecting risk behavior following elbasvir/grazoprevir treatment in patients on opioid agonist therapy: CO-STAR Part B [AASLD abstract 52]. Hepatology2018; 68(Suppl 1): 35A.
- 34. Falade-Nwulia O, Sulkowski MS, Merkow A, et al Understanding and addressing hepatitis C reinfection in the oral direct-acting antiviral era. J Viral Hepat2018; 25:220–7.
- 35. Rossi C, Butt ZA, Wong S, et al; BC Hepatitis Testers Cohort Team. Hepatitis C virus reinfection after successful treatment with direct-acting antiviral therapy in a large population-based cohort. J Hepatol2018; 69:1007–14.
- 36. Hellard M, McBryde E, Sacks Davis R, et al Hepatitis C transmission and treatment as prevention - The role of the injecting network. Int J Drug Policy2015; 26:958–62.
- 37. Martin NK, Hickman M, Hutchinson SJ, et al Combination interventions to prevent HCV transmission among people who inject drugs: modeling the impact of antiviral treatment, needle and syringe programs, and opiate substitution therapy. Clin Infect Dis2013; 57(Suppl 2):S39–45.
- 38. Turner KM, Hutchinson S, Vickerman P, et al The impact of needle and syringe provision and opiate substitution therapy on the incidence of hepatitis C virus in injecting drug users: pooling of UK evidence. Addiction2011; 106:1978–88.
- 39. Sarrazin C, Isakov V, Svarovskaia ES, et al Late relapse versus hepatitis C virus reinfection in patients with sustained virologic response after sofosbuvir-based therapies. Clin Infect Dis2017; 64:44–52.
- 40.
- 41.
- 42. Brown RS Jr, Buti M, Rodrigues L, et al Glecaprevir/pibrentasvir for 8 weeks in treatment-naïve patients with chronic HCV genotypes 1-6 and compensated cirrhosis: The EXPEDITION-8 trial. J Hepatol2020; 72:441–9.