In adults with obstructive sleep apnea (OSA) who are interested in positive airway pressure (PAP) alternatives, the multiple approaches to effective therapy may present a challenge to patients and providers when selecting a preferred treatment modality. We previously demonstrated high rates of decisional conflict and the potential for decision delay or regret in this population.
Thus, there is a need to improve patient preparedness for decision making and decision quality through better shared decision-making (SDM) processes and tools. Key components of the patient-centered SDM process include understanding patient preferences and treatment goals to enhance patient education, promote patient engagement, and align definitions of optimal outcomes.
One key contributor to decisional conflict is incomplete understanding of, or de-emphasis on, patient-defined goals for pursuing treatment. OSA treatment effectiveness is often measured by changes in disease severity via the apnea-hypopnea index (AHI) or symptom scores such as the Epworth Sleepiness Scale (ESS). However, focusing solely on these metrics does not capture patient-driven treatment goals or values (eg, cost, convenience, or recovery time), which affect adherence and efficacy. Literature regarding the treatment goals of patients with OSA, especially those seeking surgical treatment, is limited. In this study, we used a mixed methods approach to identify major treatment goal categories in adult patients with OSA. We then assessed patients’ the most important treatment goal and characterized the relationships between treatment goals and patient characteristics with a larger-scale cross-sectional survey. This information can be used to guide counseling and help patients select treatments that best meet their individual goals.
Methods
This study was approved by the Institutional Review Boards of the University of California–San Francisco (UCSF) and Kaiser Permanente Oakland.
Phase 1: Semistructured Focus Groups and Interviews—Qualitative Analysis
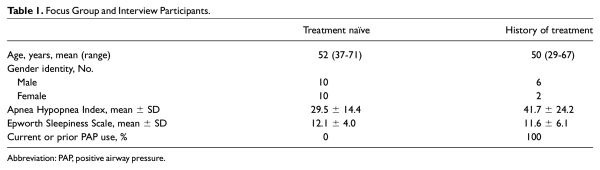
We employed a mixed methods approach, gathering data from semistructured interviews that were used to inform the design of our larger clinical survey. Methodology was in accordance with the Consolidated Criteria for Reporting Qualitative Research (Supplemental Table S1, available online). Focus groups and semistructured interviews were conducted by 2 members of the research team (P.T. and D.K.). Convenience sampling was used in recruiting participants. Adult patients newly diagnosed with OSA were recruited from Kaiser Permanente Oakland OSA education classes (treatment-naïve group). Eight 30-minute focus groups were held, with 2 or 3 participants per group. Patients with a history of OSA therapy were also recruited from the UCSF Sleep Surgery Clinic for semistructured interviews conducted individually in person or via telephone after the sleep surgery consultation (“history of treatment” group). Participants were compensated with gift cards. Recruitment was completed when themes discussed became repetitive (saturation).
Interview questions were based on prior studies examining barriers to OSA treatment and expert opinions from sleep medicine or surgery physicians at both institutions. The interview script focused on OSA symptoms, prior treatments, overall goals of treatment, and important factors when considering treatment options. During sessions, patients were encouraged to engage in conversation and introduce related topics. Following semistructured interviews, participants provided ESS scores, demographics, and AHI. Questionnaire and demographic data were documented with REDCap (Research Electronic Data Capture), a secure web-based software platform hosted at UCSF.,
Patient conversations were audio recorded and transcribed. Two investigators made field notes from transcripts and coded each one to identify key themes and ideas. Using a framework method (thematic analysis), each coder created a coding set that included collective themes that were grouped. New codes were identified from ideas that emerged in conversation, and codes were consistently revised to be more inclusive of ongoing interview themes. Each transcript was independently reviewed at least twice by each coder. As the coders became more familiar with the data, overarching themes and subthemes were identified. Saturation was achieved when no further codes were identified. Coding was done independently through Dedoose (version 8.3.47; SocioCultural Research Consultants), and coding sets were compared to ensure that no ideas were missed and to limit the discrepancies in coding style. A third investigator resolved discrepancies between coding sets and performed final analysis of transcripts to identify common themes (3 independent reviewers, 5 distinct reviews of each transcript).
Phase 2: Survey of Patients Presenting to Sleep Surgery Clinic
An electronic REDCap survey was administered to patients prior to their first consultation at the UCSF Sleep Surgery Clinic between January 2018 and October 2020. The survey queried OSA-related symptoms (ESS), PAP use, and treatment goals. Patients were asked to rate the degree to which OSA affected their daily function, using a visual analog scale (VAS-F) from 0 (no difficulty) to 100 (totally disabled). The importance of 4 common goals was queried, as based on literature, expert review, and the preceding qualitative analysis of semistructured interviews:
Your goal(s) for seeking sleep apnea treatment include: 1) To improve my daytime fatigue and feel less sleepy in the daytime, 2) To improve my snoring so those sleeping near me are not bothered by the sounds, 3) To reduce the health risks related to sleep apnea (such as heart disease and stroke), 4) To improve my sleep quality so I feel more refreshed when I wake up, and 5) Other.
Patients were asked to choose their most important primary treatment goal from the list with the option of writing in separate goals.
Medical records were reviewed for demographic and clinical data, including gender identity, age, body mass index, AHI, and ultimate pursuit of sleep surgery or related procedures (ie, drug-induced sleep endoscopy) at our institution.
Survey responses were analyzed in Microsoft Excel (version 14.5.3). ESS scores >10 represented excessive daytime sleepiness. OSA severity was based on AHI. Patients with sleep-disordered breathing and AHI <5 were included as a comparison group. Chi-square analysis compared the distribution of most important treatment goals among subgroups of patients. For comparison of treatment goals based on ESS, PAP use history, VAS-F scores, and ultimate decision to pursue surgery. Only P < .05 was used to define statistical significance.
Results
Phase 1: Semistructured Interviews
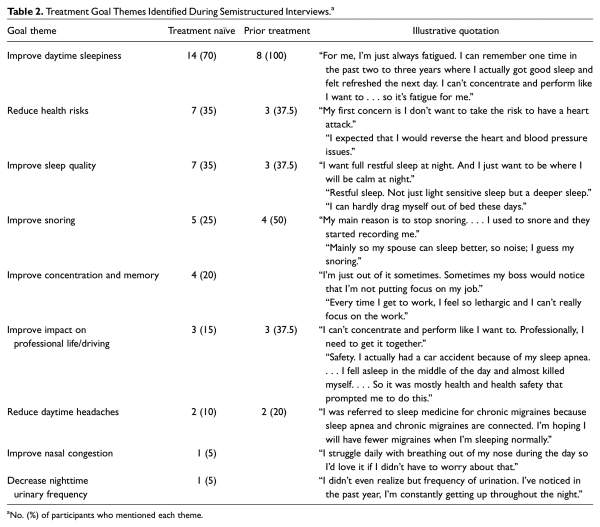
Eight focus groups with 20 patients newly diagnosed with OSA (treatment naïve) and 8 interviews with patients who had undergone prior therapy (history of treatment) were completed (Table 1). Analysis of goals for OSA therapy identified 9 subthemes (Table 2). The most common treatment goals were improving daytime sleepiness, reducing health risk with focus on cardiovascular health, improving sleep quality (depth and restfulness), and improving snoring sounds (reduction or termination).
All of the “history of treatment” group and 70% of the treatment-naïve group cited improving daytime sleepiness and fatigue as a major treatment goal. Effects of daytime sleepiness included impact on professional life, work performance, and safety while driving.
Improved health was another common treatment goal between the groups. Patients were most concerned about the cardiovascular effects of untreated OSA (“I don’t want to . . . have a heart attack”). Important sleep quality considerations included achieving more restful sleep (“not just light, sensitive sleep”), waking up feeling refreshed (“I can hardly drag myself out of bed”), and improving daytime headaches.
One-third of participants wished to reduce snoring associated with OSA, with some individuals describing this as their most important goal. Some wanted to unburden their bed partners or noted negative social pressures.
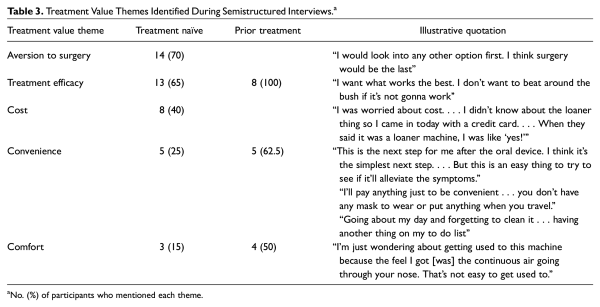
When factors or values important in treatment decisions were discussed, 5 major themes arose in both groups: efficacy, cost, convenience, comfort, and aversion to surgery (Table 3). Cost considerations were important to 50% of the treatment-naïve cohort but not mentioned by patients with history of treatment”. Convenience was a motivator (“I’ll pay anything . . . [so] you don’t have any mask to wear”). Many patients perceived PAP as burdensome (“another thing on my to do list everyday”). Treatment-naïve patients had concerns about PAP comfort (“wondering about getting used to this machine”). In the “history of treatment” group, patients shared experiences with discomfort related to PAP and oral appliance use (“very uncomfortable for my jaw and my teeth”). The majority of patients in the treatment-naïve group expressed an aversion to surgery and a desire to start with PAP therapy. However, no patients who had prior treatment shared this concern.
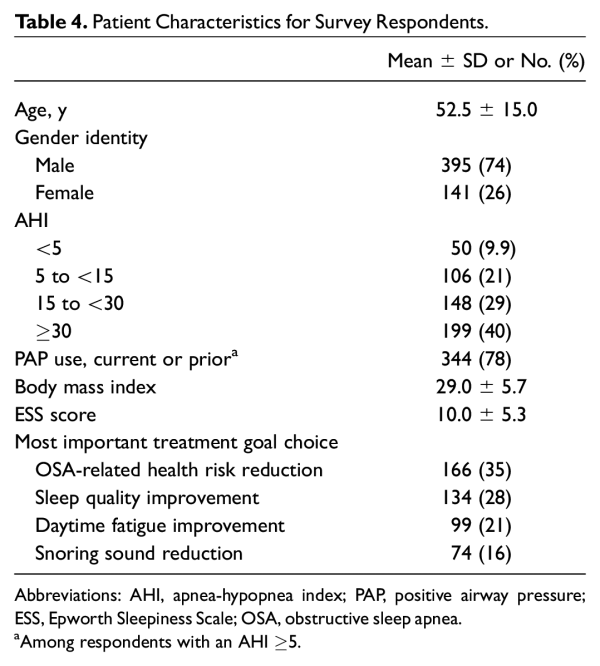
Phase 2: Survey of Patients Prior to Consultation for PAP Alternatives
A preconsultation survey was administered to 536 adult patients with a mean age of 52 years and mean AHI of 30.4 (Table 4). Among 503 patients who had a sleep study prior to their consultation, 90.1% had an AHI ≥5. Of patients with an AHI ≥5, 40% were current PAP users and 38% were previous users. When participants were asked to select any treatment goals that were important to them, 83% of respondents chose sleep quality improvement (n = 450) and OSA-related health risk reduction (n = 446). The majority also identified improvement in daytime sleepiness (73%) and reduction in snoring (65%) as important goals.
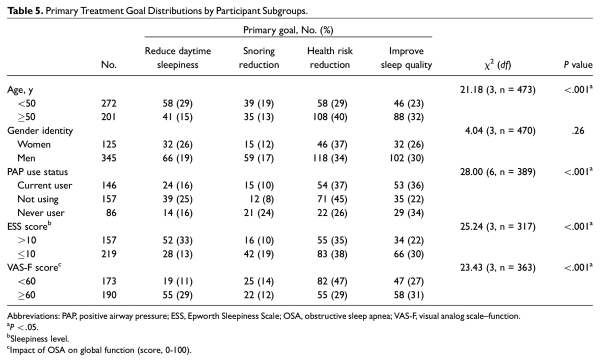
When the most important primary treatment goal was queried, health risk reduction (35%) and improving sleep quality (28%) were most frequently chosen amongst patients who completed this portion of the survey (Table 4). Primary treatment goal distributions differed by age <50 or ≥50 years (P < .0001), PAP use status (P < .0001), ESS scores (P < .0001), AHI level (P < .0001), and VAS-F scores <60 or ≥60 (P < .0001; Table 5). A higher proportion of patients with ESS scores >10 selected reduction in daytime sleepiness as their primary treatment goal than did patients with ESS scores ≤10 (P < .0001). Furthermore, a higher proportion of patients aged ≥50 years cited OSA-related health risk reduction as a primary goal than did patients aged <50 years (P = .01). Primary treatment goal distributions did not differ by gender or decision to pursue drug-induced sleep endoscopy or sleep surgery.
Post hoc comparisons of the most important treatment goal selections were performed based on OSA severity defined by AHI groups <5, 5 to <15 (mild), 15 to <30 (moderate), and ≥30 (severe). Primary treatment goal distributions differed significantly among AHI groups (P < .00001; Figure 1). Choice of health risk reduction as a primary treatment goal was selected at higher rates in those with severe OSA when compared to those with mild OSA and an AHI <5. All OSA groups chose health risk reduction at higher rates than the group with an AHI <5 (10%): mild OSA, 25% (P = .043); moderate OSA, 36% (P = .001); and severe OSA, 46% (P < .0001).
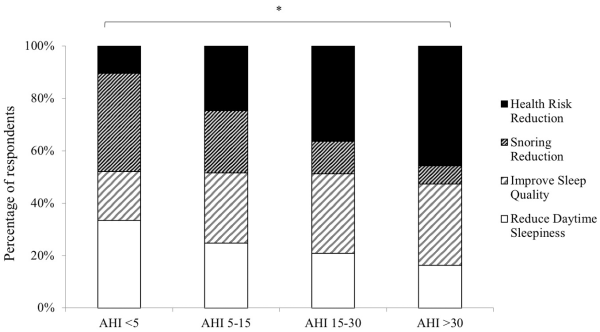
Figure 1
Primary treatment goal distributions by apnea-hypopnea index (AHI). Obstructive sleep apnea severity was associated with more patients choosing health risk reduction as their primary goal and fewer choosing snoring sound reduction. *P < .05.
In comparison, a higher proportion of the group with an AHI <5 chose snoring reduction as a primary treatment goal (38%) than patients with moderate OSA (12%, P = .0002) and severe OSA (7%, P < .00001). Similarly, a higher proportion of patients with mild OSA (24%) selected snoring reduction as most important versus patients with moderate OSA (P = .028) and severe OSA (P = .0001). No differences were found by AHI group in those who chose sleep quality or daytime sleepiness improvement as the primary goal.
A comparison of the most important treatment goal was performed by history of PAP therapy. More patients without prior PAP use selected improving sleep quality (34%), while patients who had previously used but were not currently using PAP chose reducing health risk (45%). Patients using PAP were equally interested in sleep quality improvement (36%) and health risk reduction (37%; Table 5). On analysis of patients using PAP with an AHI ≥5 (n = 118), primary treatment goals differed among the mild, moderate, and severe OSA groups (P = .0007). Of current PAP users, health risk reduction was selected as the primary treatment goal by 44% of patients with severe OSA, whereas improving sleep quality was selected by 44% of patients with moderate OSA.
Discussion
Use of SDM for patients undergoing elective surgery has been associated with reduced decisional conflict, greater patient knowledge, and improved decision quality., Improved decision quality has been linked to increased treatment compliance, reduced regret, and fewer appointment or surgery cancellations. These aspects of SDM are especially pertinent to patients presenting for sleep surgery consultation, many of whom feel that they lack adequate understanding about treatment options and have a high prevalence of decisional conflict. Despite the importance of SDM in adult OSA treatment planning, few data exist regarding treatment preferences and values in this population, especially for patients considering surgery. Alignment of patient-specific treatment goals to therapeutic options and expectations is essential in conversations about treatment recommendations. Therefore, characterizing the most important OSA treatment goals for patients is the first step in the SDM process.
In this study, we assessed patient goals and values for OSA treatment in a qualitative analysis of patients who were newly diagnosed and who had tried OSA therapies. We identified 4 main themes for treatment goals: (1) mitigation of OSA-associated health risks, (2) reduction in daytime sleepiness and fatigue, (3) improvement in sleep quality and restfulness, and (4) reduction or termination of snoring. These findings are consistent with a prior qualitative study of PAP and oral appliance users.
Our study then used goal themes to examine the most important treatment goal choice in various patient subgroups. Age (<50 or ≥50 years), PAP use, excessive daytime sleepiness (ESS score), degree of OSA impact on global function (VAS-F score), and OSA severity level were associated with differences in primary treatment goal. Notably, patients ≥50 years old were more concerned with reducing health risks than their <50-year-old counterparts, though studies on long-term effects of OSA have shown an association between age <50 years and increased all-cause mortality risk., Thus, patients aged <50 years may benefit from increased education on the health outcome implications of untreated OSA. Age may also influence perceptions of mortality.
Meanwhile, patients with severe OSA and prior (noncurrent) PAP therapy were more likely to select health risk reduction as primary goal, matching the general understanding that patients with severe and untreated OSA are at higher risk of cardiovascular morbidity than those with mild and treated OSA. Conversely, more patients who had never tried PAP cited improving sleep quality as a primary goal.
Analysis of a subset of patients who pursued drug-induced sleep endoscopy or sleep surgery did not demonstrate an association between primary treatment goals and ultimate decision to pursue these procedures. This finding has been shown in other surgical fields and is expected, as treatment goals and values may change over time and identification of patient treatment goals and values is just one component of the decision-making process.
The findings of this study can be utilized in 3 ways. First, understanding treatment goal categories aids in patient counseling. Advantages and disadvantages of treatment options should be based on the abilities of each modality to achieve or not achieve patient-specific treatment goals. This core discussion is the basis of SDM and defines treatment success that is specific and personalized.
Second, our findings identify gaps in knowledge and research needs. Comparative work is needed to understand each treatment modality’s ability to not only improve AHI but also achieve common patient treatment goals of reducing daytime sleepiness, snoring sound, and cardiovascular health risk and improving sleep quality. There is limited long-term comparative objective analysis on the ability of PAP versus oral appliances versus surgery types in reducing or terminating snoring sounds.- Similarly, data on health risk reduction with treatment are controversial. Prospective cohort studies have shown significant risks for cardiovascular morbidity and mortality in patients with OSA and risk reduction with PAP therapy.,- However, randomized controlled trials have not demonstrated measurable benefits of PAP in reducing cardiovascular risks, though duration of nightly PAP use was low in these studies., In terms of surgical outcomes, a retrospective review of >54,000 patients with OSA found that soft tissue surgery was associated with lower rates of cardiovascular, neurologic, and endocrine complications as compared with PAP; yet, no prospective controlled studies have examined surgical outcomes. Further studies of OSA treatment outcomes should align with the major patient-defined goals and expectations to allow clinicians to counsel according to factors that matter most to patients.
Third, characterization of common treatment goals is the first step in designing decision tools to help with the education and decision-making process. Treatment goals for adult OSA are often considered only in the context of objective metrics such as AHI, symptom inventories (ie, ESS), and impact on associated comorbidities. As recently noted by Malhotra et al, the chief complaint of the patient with OSA may too often be overlooked. Prior studies have demonstrated that patient and provider goals in recommending or selecting an optimal treatment frequently conflict. Thus, it is important to respect patient perspectives in consideration of treatment outcomes and incorporate these into development of SDM tools (ie, decision aids). Patient-defined treatment goals may also be used to define treatment success and, when not achieved, to serve as an impetus to consider other treatment modalities in a comprehensive approach.
This study has a few limitations. It was conducted with patients recruited from two sites within the San Francisco Bay Area. Thus, differences in findings between the treatment-naïve and “history of treatment” groups may be influenced by the disparate populations based on location. Regional and socioeconomic effects on the findings were not analyzed, limiting generalizability of the results. In addition, our survey focused on the four most commonly cited treatment goals from semistructured interviews with patients with OSA, and patients may have primary treatment goals beyond these. Future studies are needed to evaluate treatment goals specific to patients who undergo sleep surgery and to understand roles of multiple goals in surgical decision making. Future work should also investigate the influence of prior patient education and research on treatment goals and decision making.
Conclusions
Adult patients with OSA most commonly report treatment goals that can be categorized into reducing OSA-related health risks, improving sleep quality, reducing daytime sleepiness, and improving snoring. Primary treatment goal choices were associated with OSA severity, age, levels of daytime sleepiness, PAP use history, and impact of OSA on global function. Understanding and querying patient-specific goals are essential first steps in the SDM process where the conversation focuses on the ways that different treatments may or may not meet personalized goals. Ultimately, goal-focused discussions ensure alignment of priorities and definitions of success between the patient and the provider.
This article was presented at the Triological Society 123rd Annual Meeting at COSM Virtual Sessions; April 7-11, 2021.
The contents do not represent the views of the US Department of Veterans Affairs or those of the US government.
Authors’ Note Jolie L. Chang is now affiliated to Surgery Service, Department of Veterans Affairs Medical Center, San Francisco, California, USA.
Author Contributions Yi Cai, data collection, data analysis and interpretation of results, manuscript preparation; Priyanka Tripuraneni, data collection, data analysis and interpretation of results, manuscript preparation; Arushi Gulati, data collection, data analysis and interpretation of results, manuscript preparation; Erika M. Stephens, data collection, data analysis and interpretation of results; Dang-Khoa Nguyen, data collection, data analysis and interpretation of results; Megan L. Durr, study design and supervision, manuscript preparation; Jolie L. Chang, study design, data collection and interpretation, supervision, manuscript preparation.
Disclosures Competing interests: None.
Disclosures Sponsorships: None.
Disclosures Funding source: This project was supported by the Mount Zion Health Fund. Jolie L. Chang is supported by the Veterans Affairs Medical Center, San Francisco, California.
Supplemental Material Additional supporting information is available in the online version of the article.
References
- 1. Gulati A, Stephens EM, Cai Y, Chang JL. Characterizing decisional conflict in patients presenting to sleep surgery clinic and an exploration of resource limitations. Laryngoscope. 2021;131(10):2384–2390.
- 2. Hilbert J, Yaggi HK. Patient-centered care in obstructive sleep apnea: a vision for the future. Sleep Med Rev. 2018;37:138–147.
- 3. Tariq S, Woodman J. Using mixed methods in health research. JRSM Short Rep. 2013;4:2042533313479197.
- 4. Tong A, Sainsbury P, Craig J. Consolidated Criteria for Reporting Qualitative Research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–357.
- 5. Elfil M, Negida A. Sampling methods in clinical research: an educational review. Emerg (Tehran). 2017;5:e52.
- 6. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381.
- 7. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
- 8. Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117.
- 9. Boss EF, Mehta N, Nagarajan N, et al. Shared decision making and choice for elective surgical care: a systematic review. Otolaryngol Head Neck Surg. 2016;154:405–420.
- 10. Fowler FJ Jr, Gallagher PM, Drake KM, Sepucha KR. Decision dissonance: evaluating an approach to measuring the quality of surgical decision making. Jt Comm J Qual Patient Saf. 2013;39:136–144.
- 11. Sun Q. Predicting Downstream Effects of High Decisional Conflict: Meta-analyses of the Decisional Conflict Scale. University of Ottawa; 2005.
- 12. Barry MJ, Edgman-Levitan S. Shared decision making—the pinnacle of patient-centered care. N Engl J Med. 2012;366:780–781.
- 13. Almeida FR, Henrich N, Marra C, et al. Patient preferences and experiences of CPAP and oral appliances for the treatment of obstructive sleep apnea: a qualitative analysis. Sleep Breath. 2012;17:659–666.
- 14. Rich J, Raviv A, Raviv N, Brietzke SE. All-cause mortality and obstructive sleep apnea severity revisited. Otolaryngol Head Neck Surg. 2012;147:583–587.
- 15. Lavie P, Lavie L, Herer P. All-cause mortality in males with sleep apnoea syndrome: declining mortality rates with age. Eur Respir J. 2005;25:514–520.
- 16. Cicirelli VG. Fear of death in mid-old age. J Gerontol B Psychol Sci Soc Sci. 2006;61:P75–P81.
- 17. Marin JM, Carrizo SJ, Vicente E, Agusti AGN. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–1053.
- 18. Lee CN, Hultman CS, Sepucha K. Do patients and providers agree about the most important facts and goals for breast reconstruction decisions? Ann Plast Surg. 2010;64:563–566.
- 19. Li H-Y, Lin Y, Chen N-H, Lee L-A, Fang T-J, Wang P-C. Improvement in quality of life after nasal surgery alone for patients with obstructive sleep apnea and nasal obstruction. Arch Otolaryngol Head Neck Surg. 2008;134:429.
- 20. Li H-Y. Palatal surgery for obstructive sleep apnea. Sleep Med Clin. 2019;14:51–58.
- 21. Robinson S, Chia M, Carney AS, Chawla S, Harris P, Esterman AE. Upper airway reconstructive surgery long-term quality-of-life outcomes compared with CPAP for adult obstructive sleep apnea. Otolaryngol Head Neck Surg. 2009;141:257–263.
- 22. Gotsopoulos H, Chen C, Qian J, Cistulli PA. Oral appliance therapy improves symptoms in obstructive sleep apnea. Am J Respir Crit Care Med. 2002;166:743–748.
- 23. Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease. Am J Respir Crit Care Med. 2001;163:19–25.
- 24. Doherty LS, Kiely JL, Swan V, McNicholas WT. Long-term effects of nasal continuous positive airway pressure therapy on cardiovascular outcomes in sleep apnea syndrome. Chest. 2005;127:2076–2084.
- 25. Buchner NJ, Sanner BM, Borgel J, Rump LC. Continuous positive airway pressure treatment of mild to moderate obstructive sleep apnea reduces cardiovascular risk. Am J Respir Crit Care Med. 2007;176:1274–1280.
- 26. McEvoy RD, Antic NA, Heeley E, et al. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med. 2016;375:919–931.
- 27. Sánchez-de-la-Torre M, Sánchez-de-la-Torre A, Bertran S, et al. Effect of obstructive sleep apnoea and its treatment with continuous positive airway pressure on the prevalence of cardiovascular events in patients with acute coronary syndrome (ISAACC study): a randomised controlled trial. Lancet Respir Med. 2020;8:359–367.
- 28. Ibrahim B, de Freitas Mendonca MI, Gombar S, Callahan A, Jung K, Capasso R. Association of systemic diseases with surgical treatment for obstructive sleep apnea compared with continuous positive airway pressure. JAMA Otolaryngol Head Neck Surg. 2021;147:329–335.
- 29. Evans EC, Sulyman O, Froymovich O. The goals of treating obstructive sleep apnea. Otolaryngol Clin North Am. 2020;53:319–328.
- 30. Malhotra A, Nokes B, DeYoung P, Owens R. Why do we sometimes ignore the chief complaint in patients evaluated for obstructive sleep apnea? J Clin Sleep Med. 2020;16:657–659.