Introduction
Lichen planus pigmentosus (LPP) is a distinct clinical entity commonly encountered in the Indian population. It is characterized by insidious onset of blue-brown macules over the sun-exposed areas and the flexures. The lesions of LPP are usually asymptomatic, although some lesions may be associated with pruritus or a burning sensation. However, cosmetically, it is bothersome. There is no standard treatment for this condition. Various therapeutic modalities like topical tacrolimus, systemic corticosteroids, and lasers have been tried with varying success. Isotretinoin has been tried previously and had been found to be effective in LPP. Herein, we report a case series of 10 patients who showed good response to combination of oral isotretinoin (20 mg/day) and topical 0.1% tacrolimus ointment.
Case Series
Ten patients with clinical and histopathological diagnosis of LPP who were treated with combination of oral isotretinoin (20 mg/day) and topical 0.1% tacrolimus ointment twice daily have been reported in this case study. All patients were recruited after getting a written informed consent. Demographic and clinical details are given in Table 1. Patients between ages 20 and 62 years were included in this study. The minimum duration of symptoms at the time of presentation was 3 month and the maximum duration was 36 months. In this study, at the time of presentation all patients had a progressive disease. Clinical examination showed that well to ill-defined dark brown or bluish gray macules irregular in shape with irregular borders were merging at places to form large patches over neck and face (patches over neck and face = seven cases, patches over face = three cases) [Figure 1A and C]. Among the morphologic variants of LPP, diffuse type was seen in all the patients. Baseline investigations were normal and repeat liver function tests and serum lipid profile after 1 month were also normal. Urine pregnancy test was negative in all the females. Improvement in the pruritus was seen as early as 2 weeks of treatment. Stabilization of the disease activity was observed by 4 to 5 weeks. An appreciable decrease in hyperpigmentation was identified after 8 weeks of regular treatment. Seven patients had 25% to 50% improvement in hyperpigmentation, while three patients had >50% response. The maximum reduction in hyperpigmentation was 75% seen in two out of three patients with >50% response; however, none of our patients had complete clearance in pigmentation at the end of 3 months [Figure 1B and D]. The drug was well tolerated in all except one patient, who developed deranged lipid profile, which was well controlled with antilipidemic medication. Minimal adverse events in the form of mild cheilitis (n = 3), xerosis (n = 2), and transient transaminitis (n = 2) were observed, which did not warrant discontinuation of treatment.
Table 1
Clinicoepidemiological profile of patients with LPP
| Sr. no. | Age (year/sex) | Duration (months) | Symptoms | Precipitating factors | Previous treatment | Improvement in pigmentation (response) |
|---|---|---|---|---|---|---|
| 1 | 23/M | 6 | Pruritus | Mustard oil | Undocumented | Moderate |
| 2 | 45/M | 18 | Cosmetic | Hair dye and mustard oil | Topical steroids | Good |
| 3 | 62/F | 36 | Pruritus | Mustard oil | Triple combination depigmenting cream and sunscreen | Moderate |
| 4 | 36/F | 24 | Cosmetic | Nil | Depigmenting agents | Moderate |
| 5 | 55/M | 12 | Cosmetic | Nil | Undocumented | Good |
| 6 | 49/F | 3 | Cosmetic | Cosmetic product | Undocumented | Moderate |
| 7 | 38/F | 24 | Pruritus | Hair dye | Tacrolimus 0.1% ointment | Good |
| 8 | 59/F | 14 | Asymptomatic | Hair dye | Undocumented | Moderate |
| 9 | 20/M | 7 | Cosmetic | Hair dye | Undocumented | Moderate |
| 10 | 40/F | 6 | Cosmetic | Hair dye | Undocumented | Moderate |
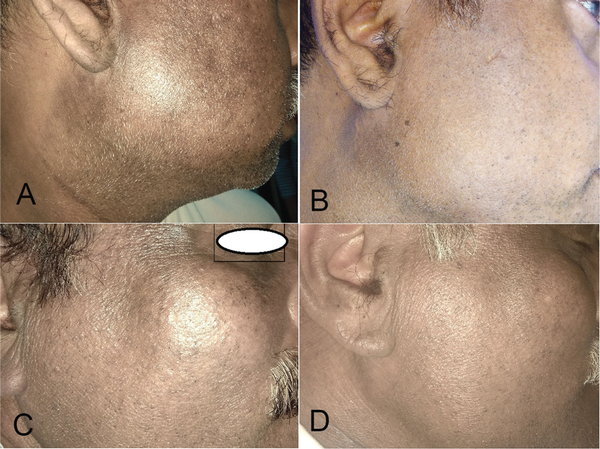
Figure 1
(A and C) Ill-defined dark brown or slate gray macules over mandibular area and side of neck before treatment. (B and D) Reduction of the pigmentation after 3 months of treatment.
Discussion
Even 40 years after its initial description, treatment of LPP is generally unsatisfactory. Topical tacrolimus, a specific suppressor of T cell-mediated inflammation has been considered a reasonable treatment option. A study by Al-Mutairi and El-Khalawany showed beneficial role of tacrolimus ointment (twice daily application for the duration varying from 6–2 weeks) in 13 patients of LPP. Out of these 13 patients, seven (53.8%) patients showed appreciable lightening of the pigmentation after an average of 12 weeks. Isotretinoin with its anti-inflammatory properties has been reported to be effective in LPP; however, its role in LPP is yet to be further elucidated. The possible mechanism of action of isotretinoin in LPP is anti-inflammatory and immunomodulatory action. In a prospective study (32 patients of LPP) by Muthu et al., moderate improvement (26%–50%) in hyperpigmentation was observed in nearly half of the patients and good improvement (50%) was seen in one-fifth of the patients treated with 20 mg of isotretinoin and sunscreen for a period of 6 months. Here it means that isotretinoin 20mg is given for 6months and response of treatment of started in intially 4 to 6 weeks means improvement noticed and disease was stabilize. In our study, appreciable decrease in hyperpigmentation was identified after 8 weeks of regular treatment. Seven patients had 25% to 50% improvement in hyperpigmentation, while three patients had >50% response. The maximum reduction in hyperpigmentation was 75% seen in two out of three patients with >50% response. In a case of recalcitrant LPP, treated by oral isotretinoin 20 mg daily, significant improvement in hyperpigmentation was observed after 2 months of treatment and stabilization of disease with no new lesions was achieved after 3 months of treatment. Further, after 9 months of treatment, the patient had dramatic improvement from her pretreatment appearance with near-complete resolution of her bluish gray dyschromia over face and at other sites. In our study, seven patients had 25% to 50% improvement in hyperpigmentation while none of our patients had complete clearance in pigmentation at the end of 3 months. Verma and Pandhi successfully used a combination of topical 0.1% tacrolimus and oral dapsone in five LPP patients. In a 32-year-old male with widespread LPP, treated with clobetasol dipropionate 0.05% ointment, tacrolimus 0.1% ointment, and low-dose isotretinoin (0.1–0.2 mg/kg/day), decrease in the progression and hyperpigmentation of patches was observed after 6 months [Table 2]. A combination of two therapeutic modalities may be more effective in terms of quicker and better response. With this assumption, we had tried this combination of topical tacrolimus 0.1% and oral isotretinoin and found it to be efficacious and safe. Symptomatic improvement in pruritus was seen as early as 2 weeks after treatment, followed by stabilization of disease in another 2 to 3 weeks. This was followed by appreciable lightening of pigmentation in next 4 weeks. Duration of treatment was only 3 months as against 6 months in previous studies where isotretinoin was used. We could not follow up the patients regularly after this because of current COVID-19 pandemic. Prolongation of this treatment might have shown an even better response.
Table 2
Previously used treatments in LPP
| Authors | Patients | Durations | Treatment given | Response |
|---|---|---|---|---|
| Al-Mutairi and El-Khalawany | 13 | 6–12 weeks | Topical tacrolimus 0.03% | 7 (53.8%) patients showed appreciable lightening of the pigmentation after an average of 12 weeks |
| Muthu et al. | 32 | 6 months | 20 mg/day oral isotretinoin | Moderate improvement (26%–50%) in hyperpigmentation was observed in nearly half of the patients and good improvement (50%) was seen in one-fifth of the patients after 6 months |
| Shah et al. | 1 | 12 months | 20 mg/day oral isotretinoin | Stabilization of the disease with no new lesions was achieved after 3 months of treatment. After 9 months of treatment, the patient had dramatic improvement from her pretreatment appearance with near-complete resolution of her bluish gray dyschromia over face and at other sites |
| Lee et al. | 1 | 6 months | Topical 0.1% tacrolimus, clobetasol dipropionate 0.05%, and low-dose isotretinoin 0.1–0.2 mg/kg/day | Decrease in the progression and hyperpigmentation of patches was observed after 6 month |
Conclusion
To the best of our knowledge, this is the first case series demonstrating the efficacy of combination of topical tacrolimus 0.1% and oral isotretinoin in stabilizing and decreasing the hyperpigmentation in LPP, particularly in patients having limited disease of short duration. We propose this combination as an effective and safe treatment for this difficult to treat and cosmetically disabling pigmentary disorder. However, prospective studies with longer duration of treatment and prolonged follow-up period are required to confirm our observations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1
Al-Mutairi N, El-Khalawany M. Clinicopathological characteristics of lichen planus pigmentosus and its response to tacrolimus ointment: an open label, non-randomized, prospective study. J Eur Acad Dermatol Venereol 2010;24:535-40.2
Munoz-Perez MA, Camacho F. Pigmented and reticulated plaques of folds. A case of lichen planus pigmentosus-inversus? Eur J Dermatol 2002;12:282.3
Ohshima N, Shirai A, Saito I, Asahina A. Lichen planus pigmentosus-inversus occurring extensively in multiple intertriginous areas. J Dermatol 2012;39:412-4.4
Kim JE, Won CH, Chang S, Lee MW, Choi JH, Moon KC. Linear lichen planus pigmentosus of the forehead treated by neodymium: yttrium-aluminum-garnet laser and topical tacrolimus. J Dermatol 2012;39:189-91.5
Woo TY. Systemic isotretinoin treatment of oral and cutaneous lichen planus. Cutis 1985;35:385-6.6
Cribier B, Frances C, Chosidow O. Treatment of lichen planus. An evidence-based medicine analysis of efficacy. Arch Dermatol 1998;134:1521-30.7
Sehgal VN, Verma P, Bhattacharya SN, Sharma S, Rasool F. Lichen planus pigmentosus. Skinmed 2013;11:96-103.8
Muthu SK, Narang T, Saikia UN, Kanwar AJ, Parsad D, Dogra S. Low-dose oral isotretinoin therapy in lichen planus pigmentosus: an open-label non-randomized prospective pilot study. Int J Dermatol 2016;55:1048-54.9
Shah P, Ugonabo N, Liebman T. A case of recalcitrant lichen planus pigmentosus treated by oral isotretinoin. JAAD Case Rep 2020;6:812-4.10
Verma P, Pandhi D. Topical tacrolimus and oral dapsone combination regimen in lichen planus pigmentosus. Skinmed 2015;13:351-4.11
Lee N, Manalili FH, Dayrit J. Widespread lichen planus pigmentosus in a 32-year-old Filipino male treated with low dose isotretinoin and topical tacrolimus. J Phil Dermatol Soc 2019;29:122-4.
