Introduction
There is no evidence-based, theoretically driven, and psychological intervention specifically for harmful grandiose delusions. Indeed, grandiose delusions are often overlooked in the treatment of psychosis. Partly this may be because the belief content can seem benign compared to other psychotic experiences. However, qualitative interviews with patients with these beliefs indicate that problematic burdens, responsibilities, and behaviors are often inherent in the belief systems (eg, believing one is Jesus and feeling under pressure to save humanity). Shared recognition by patients and clinicians of such difficulties could form the basis of engagement in treatment. Recently, we outlined how the multiple meanings obtained from grandiose delusions may be a key reason why the beliefs persist despite the associated difficulties. Yet there are also other plausible factors—for instance, immersion within the grandiose identity and too much time thinking about the beliefs—that may help explain why grandiosity endures and problems result. In this article, we aim to develop an understanding of the types and prevalence of difficulties following grandiose delusions; why the delusions may persist and harmful consequences result; and the factors associated with patients wanting help.
Grandiosity is associated with lower patient motivation to engage in standard mental health treatment. This likely results from interactions with services that do not provide patients with a suitable rationale for engagement. Engagement might be enhanced if clinicians are able to ask knowledgeably about the different types of problems—often fairly subtle—that grandiose delusions bring in their wake. In a qualitative study, patients with experience of grandiose delusions described difficulties occurring across multiple domains including physical (eg, trying to fly), sexual (eg, going home with strangers believing them to be God), social (eg, rejection by others), emotional (eg, feeling suicidal), and occupational (eg, dropping out of university). We, therefore, wanted to develop a measure that could capture these harms.
Several factor analytic studies of psychotic experiences show that there is a single dimension of grandiosity in the general population. This suggests that there are unlikely to be different types of grandiose delusions in clinical presentations. Indeed, factor analyses cutting across diagnostic categories demonstrate grandiosity continuing to load on a single dimension. Furthermore, characteristics of grandiose delusions (conviction, pervasiveness, preoccupation, action, inaction, an negative affect) have been found to load onto the same factor structure across bipolar and schizophrenia diagnostic categories. The understanding of factors that maintain grandiose delusions specifically is in its infancy. The meaning of the delusions, reasoning biases, and associated hallucination content are possible maintenance factors.,, We highlight 2 further potential factors that patients have reported to us. Immersion behaviors are when individuals take actions in line with their grandiose beliefs, which includes acting according to the perceived identity (eg, blessing people believing that one is Jesus). Such behaviors might provide compelling memories that provide confirmatory evidence for the belief. Furthermore, individuals may withdraw from others and become engrossed in information linked to their belief (eg, researching the second coming of Christ online) potentially reducing access to disconfirmatory evidence and providing further confirmatory evidence. A second potential driver is an excessive time spent thinking about the belief. Patients describe thinking about their grandiose beliefs “all the time”, having difficulty stopping such thoughts, and experiencing verbal and imagery-based repetitive thinking. Such thoughts are often pleasurable which may partially explain their perseverative nature, but they may also be driven by the belief’s meaning (eg, it might feel important to focus on how one will save humanity, even if it is stressful rather than pleasurable to do so). It seems probable—akin to worry in persecutory delusions—that such repetitive thinking can drive grandiose beliefs by bringing the belief to mind, elaborating its details, and increasing conviction. Consistent with this hypothesis, a study with 109 nonclinical participants found that compared to distraction, rumination on a positive memory was associated with the maintenance of grandiose ideation. Additionally in both groups with a bipolar I diagnosis (n = 27) and nonclinical individuals (n = 27), compared to “distanced reflection”, an immersive rumination on a positive memory was associated with increased number of positive thoughts. It has yet to be investigated in a clinical population whether repetitive thinking specifically about grandiose beliefs is associated with higher levels of grandiosity and degree of conviction.
The study aims were to: (1) determine the extent to which patients identify difficulties arising from their grandiose delusions, (2) assess the extent to which they engage in immersion behaviors and repetitive thinking about their grandiose delusions, and whether these processes are associated with higher levels of grandiosity and subjective harm, and (3) determine factors associated with patients wanting help.
Methods
Study Design and Participants
The NHS Health Research Authority South Central Oxford C Research Ethics Committee (20/SC/0430) and University of Oxford Central University Research Ethics Committee (R69315/RE001) provided ethical approval. We conducted a cross-sectional questionnaire study with 2 cohorts. In the clinical cohort, participants were recruited from 39 NHS mental health trusts across England and Wales. Inclusion criteria were: Aged 16+ years, accessing adult secondary care NHS mental health services, and being diagnosed with non-affective or affective psychosis. Exclusion criteria were insufficient English language to participate or primary diagnosis of alcohol/drug disorder, personality disorder, or organic syndrome. Participants provided informed consent and data were collected in person or online via Qualtrics. The nonclinical cohort was recruited via social media advertisements. Inclusion criteria were: Aged 18+ years, having internet access, and UK/ROI nationality/residence. There were no exclusion criteria. Participants provided informed consent online. Data were collected using Qualtrics.
Assessment Measures
Grandiosity
The specific psychotic experiences questionnaire-grandiosity subscale (SPEQ-G) is a self-report measure of grandiosity with good psychometric properties. Respondents indicate how much they agree with eight statements (eg, “I am or am destined to be someone very important”) for the last month on a 4-point Likert scale (0–3). Higher scores indicate higher levels of grandiosity. The internal reliability of the scale was satisfactory (Cronbach’s α = .72) and good (Cronbach’s α = .81) in the nonclinical and clinical cohorts, respectively.
The SPEQ-G was used to identify participants scoring highly enough in grandiosity for administration of the item pools. The cutoff was ≥5, consistent with Isham et al (corresponding to the top 15th percentile scores in a nonclinical sample). To identify the grandiose belief explicitly, those scoring above the threshold were asked for a brief description of their specific experience of having exceptional abilities, identity, role, mission, or wealth (eg, “I am on a special mission from God to save the world”) and to rate belief conviction (0–100%). Instructions specified that subsequent measures should be answered in relation to this content. In the clinical group, participants were supported by clinical studies officers who had received training on eliciting grandiose delusions.
Subjective Harm, Immersion Behaviors, and Repetitive Thinking
We developed item pools for the subjective harm from exceptional experiences questionnaire (SHEEQ), immersion behaviors questionnaire-exceptional experiences (IBQ-EE), and thinking about exceptional experiences questionnaire (TEEQ). Items were generated using deductive and inductive methods via revisiting patient descriptions from our previous qualitative study, review of the wider relevant literature, and consultation with experts in the field including our patient advisory group with lived experience of grandiose delusions, and clinical psychologists and psychiatrists specializing in psychosis. The initial item pools had 9, 22, and 7 items, respectively, with answers given on a 5-point Likert scale (0 = not at all/none of the time and 4 = all of the time; Supplementary tables S1–S3). The 9 SHEEQ items asked about harm in the last 6 months, but participants were also asked 2 lifetime harm questions. These items did not contribute to the SHEEQ total score, but the latter (“Is this something you have ever wanted help with?”) was used to measure wanting help. The TEEQ was administered in clinical and nonclinical groups. The SHEEQ and IBQ-EE were only administered to the clinical group as these required a clearly specified grandiose delusion.
Analysis
Analyses were conducted in R version 4.0.3 (packages: “psych” version 2.0.9, “lavaan” version 0.6-9). For measure development, prior to factor analysis, Bartlett’s Test of Sphericity and the Kaiser–Meyer Olkin Measure of Sampling Adequacy (KMO) were used to assess the feasibility of factor recovery based on the observed dataset. Parallel analysis based on polychoric correlations (assuming ordinal data) were used to identify the number of factors to retain. Retention of factors was based on comparisons between the eigenvalues of the observed data and random data.
Cohorts were randomly split into 2 subsamples, enabling item pool refinement using exploratory factor analysis (EFA) and a test of the factor structure using confirmatory factor analysis (CFA). For the SHEEQ and IBQ-EE analyses, the first and second subsamples had 151 and 211 clinical participants, respectively. For the TEEQ analysis, data from the nonclinical and clinical cohorts were combined. The first subsample comprised 699 nonclinical and 122 clinical participants and the second comprised 700 nonclinical and 236 clinical participants. More clinical participants were included in the second subsample to ensure sufficient numbers for measurement invariance analysis (used to assess whether the measure performed similarly across the nonclinical and clinical groups).
Psychometric properties were assessed using ordinal alpha for internal consistency, and intraclass correlations for 1-week test–retest reliability.
We assessed the extent to which immersion behaviors and thinking about exceptional experiences were associated with the degree of grandiosity, grandiose belief conviction, and subjective harm, and which factors were associated with wanting help. Pair-wise associations were tested using Pearson’s correlations, using factor scores for latent variables and raw scores for grandiose belief conviction and wanting help. Structural equation modeling delivered prediction models incorporating multiple predictors. For the tests of association, 352 participants provide >95% power to detect a Pearson’s correlation coefficient of 0.2 at a 5% significance level. Supplementary materials provide further methodological details.
Results
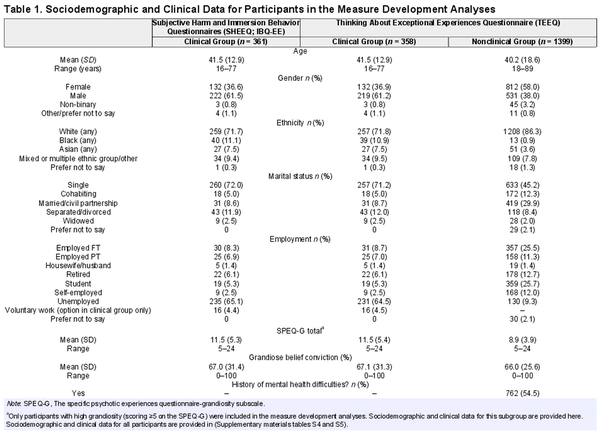
Sociodemographic information for participants included in the measure development analyses (ie, those with high grandiosity) is summarized in table 1. Supplementary tables S4 and S5 provide information for the full sample.
Part 1: Measure Development
Subjective Harm (SHEEQ):
Bartlett’s test of sphericity and KMO tests indicated that factor analysis was appropriate for the first subsample [χ2(36) = 870.13, P < .0001; KMO = 0.83]. Following parallel analysis and model comparison, a one-factor solution was determined best. No items were removed, and all had a factor loading of >0.4. The 9-item one-factor model after EFA explained 49.7% of the variance. Supplementary table S6 provides factor loadings. CFA in the second subsample showed that the 9-item one-factor model had fit indices: Robust-χ2(27) = 80.993, CFI = 0.973, TLI = 0.964, RMSEA = 0.098, SRMR = 0.059. Whilst these were predominantly good, the RMSEA was above the acceptable threshold, so post hoc analysis was conducted evaluating model adequacy based on the modification index. This indicated that the residuals of items H7 and H8 were correlated (see Supplementary materials). After incorporating this correlation into the model, the final 9-item one-factor model had acceptable fit indices: Robust-χ2(26) = 53.535, CFI = 0.986, TLI = 0.981, RMSEA = 0.071, SRMR = 0.054. Supplementary table S7 provides factor loadings. The SHEEQ had excellent internal consistency (ordinal α = 0.92). One hundred and thirty-three participants provided follow-up data within 3 to 10 days (mean = 7.29, SD = 1.29). The intraclass correlation was 0.68 indicating good test–retest reliability.
Immersion Behaviors (IBQ-EE):
Bartlett’s test of sphericity and KMO tests indicated that factor analysis was appropriate for the first subsample [χ2(231) = 2422.826, P < .0001; KMO = 0.88]. Parallel analysis indicated that a multiple-factor model may be appropriate but as the largest eigenvalue was 7.5 times the size of the next largest, the possibility of a simple one-factor solution was also considered. We conducted a model comparison to determine the most appropriate solution and, given that our a priori intention was to provide a uni-dimensional measure that could capture any potential variances at a factor level, we compared exploratory bifactor models based on 2-, 3-, and 4-factor solutions (rather than simple correlated factor models) to the one-factor solution. Ultimately, the simple one-factor solution was considered the most appropriate. Although the more complex bifactor models explained slightly more of the variance in the data, there was substantial cross-loading of items which would have necessitated removing several clinically valuable items. In the one-factor solution, all items loaded with a value >0.4. The 22-item one-factor solution explained 40.8% of the variance (Supplementary table S6 provides factor loadings).
CFA in the second subsample showed that the 22-item one-factor model derived from the EFA had fit indices: Robust-χ2(209) = 527.514; CFI = 0.911, TLI = 0.901; RMSEA = 0.085; SRMR = 0.087. These were on the boundary of acceptability. To improve fit further we conducted a post hoc analysis evaluating model adequacy based on the modification index. This indicated that residuals from 2 pairs of items were correlated and these associations were added to the model. This final model had a marginally high SRMR but as all other fit indices were comfortably in the acceptable range, and we report robust rather than standard indices, it was considered the model had an acceptable fit: Robust-χ2(207) = 467.536; CFI = 0.927, TLI = 0.919; RMSEA = 0.078; SRMR = 0.082 (Supplementary table S7 provides factor loadings). The IBQ-EE had excellent internal consistency (ordinal α = 0.95). 133 participants provided follow-up data within 3 to 10 days (mean = 7.29, SD = 1.29) and the intraclass correlation (ICC = 0.76) indicated good test–retest reliability.
Perseverative Thinking (TEEQ):
Bartlett’s test of sphericity and KMO tests indicated that factor analysis was appropriate for the first subsample [χ2(21) = 5100.51, P < .0001; KMO = 0.90]. Parallel analysis and model comparison indicated that 1- or 2-factor solutions were viable, but the 2-factor solution (“thinking a lot” and “difficulty controlling thoughts”) was considered the most appropriate theoretically. These are arguably related but not synonymous constructs (a person might think about their perceived role as a SAS operative repetitively, not because they cannot control the thoughts, but because it feels important to do so). The factor correlation between the 2 factors was 0.71, supporting the idea of these as distinct albeit strongly related constructs. Following the criteria for item removal, one item was considered for removal (Q5 “It has been hard to think about anything else”) due to cross-loading. We decided to retain it, however, as theoretically it matched well with the “difficulty controlling thoughts” factor, had clinical utility, and could be removed at CFA stage if still problematic. Therefore, all items remained following EFA and the final 7-item 2-factor model explained 78.0% of the variance in the data (Supplementary table S6 shows factor loadings).
CFA in the second subsample showed that the 7-item, 2-factor model derived from the EFA had fit indices: Robust-χ2(13) = 304.367; CFI = 0.980, TLI = 0.968; RMSEA = 0.155; SRMR = 0.045. The high RMSEA indicated poor fit so we conducted post hoc analysis, evaluating model adequacy based on the modification index. This demonstrated that the residuals of Q6 and Q7, and Q1 and Q2 were correlated. When these associations were added to the model, the fit indices indicated an excellent fit to the data (robust-χ2(11) = 48.051; CFI = 0.997, TLI = 0.995, RMSEA = 0.060, SRMR = 0.018; Supplementary table S7 provides factor loadings). The factor correlations in the CFA sample were very high (0.94), and therefore we ran the CFA again post hoc, first with a one-factor model and then with a bifactor model with one general and 2 specific factors to see whether either provided a better solution. The one-factor model had a poor fit to the data as the RMSEA was very high [robust-χ2(14) = 548.215, CFI = 0.964, TLI = 0.946, RMSEA = 0.202, SRMR = 0.071] and to achieve an adequate fit many pairs of residuals had to be correlated. The bifactor model failed to converge. Therefore, we retained the original 2-factor solution.
We tested across 4 levels of measurement invariance. Changes in CFI and RMSEA were within the acceptable threshold, indicating that the TEEQ performs similarly in the nonclinical and clinical groups (Supplementary table S8). Comparisons of latent factor mean between these groups are therefore valid, and these were significantly higher in the clinical group than the nonclinical group.
The TEEQ had good internal consistency (ordinal alphas were 0.91 and 0.88 for “thinking a lot” and “difficulty controlling thoughts”). A total of 338 participants (227 from the nonclinical group and 111 from the clinical group) provided follow-up data within 7 to 10 days (mean = 7.58, SD = 0.86). Test–retest reliability was good (ICCs were: 0.76 for “thinking a lot” and 0.72 for “difficulty controlling thoughts”).
Part 2: Item Endorsement in the Grandiose Delusion Clinical Group
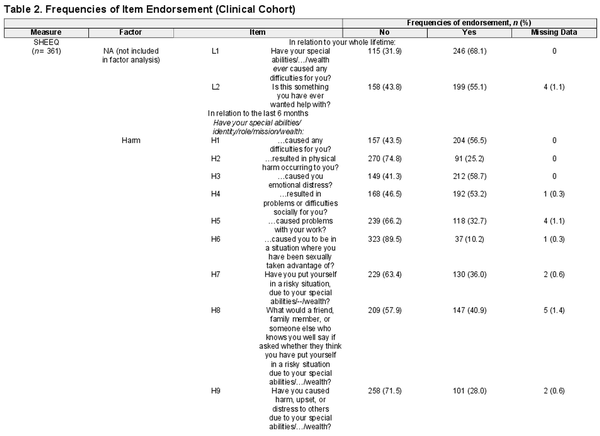
To describe how frequently clinical participants endorsed items on each measure, we dichotomized responses to “not endorsed” or “endorsed” (see table 2, and for non-dichotomized responses Supplementary tables S9–S11). 77.9% (268/344) of patients endorsed at least 1 item of harm as occurring in the past 6 months. This rose to 84.6% (291/344) for lifetime occurrence. Even when removing item H8, which asks about whether others think the person has put themselves at risk, endorsement rates remained high: 75.6% (260/344) endorsed at least 1 item for the past 6 months, and 83.7% (288/344) for lifetime occurrence. Participants typically endorsed 5 of the 11 harm items (mean = 4.67, SD = 3.28). The most endorsed domains were emotional distress (58.7%, 212/361) and social problems (53.2%, 192/361). 28.0% (101/361) of patients thought that their experience had caused harm to others. 55.1% (199/361) said they had wanted help with difficulties arising from their grandiose belief.
In total, 92.6% (326/352) of participants endorsed using at least one immersion behavior in the past month, with the average number being 8 of 22 items (mean = 8.21, SD = 5.66). The 3 most commonly endorsed items were: “acted in relation to your special abilities/identity/role/mission/wealth in private” (63.4%, 229/361); “withdrawn from others to explore, understand, or immerse yourself in your special abilities/identity/role/mission/wealth” (54.3%, 196/361); and “spent time researching or finding information that relates to your special abilities/identity/role/mission/wealth” (52.6%, 190/361).
In total, 89.1% (319/358) of patients endorsed at least one of the thinking about exceptional experiences items. Participants endorsed a mean of 2.86 of the 4 “thinking a lot” items (SD = 1.46) and 1.53 of the 3 “difficult to control” items (SD = 1.20). Endorsement rates for “thinking a lot” items (66.2–77.7%) were higher than for “difficulty controlling thoughts” items (45.0–56.4%).
Part 3: Tests of Associations With Grandiosity in the Clinical Group
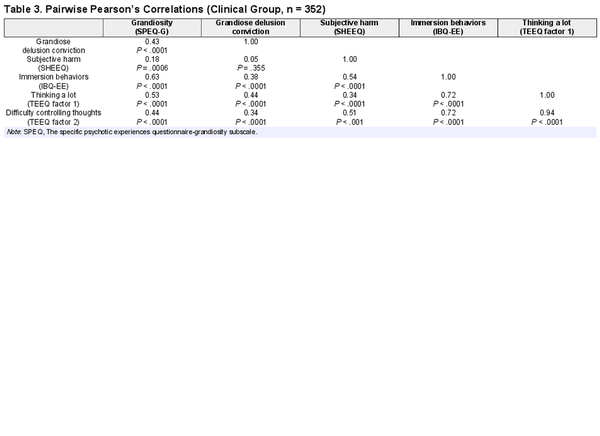
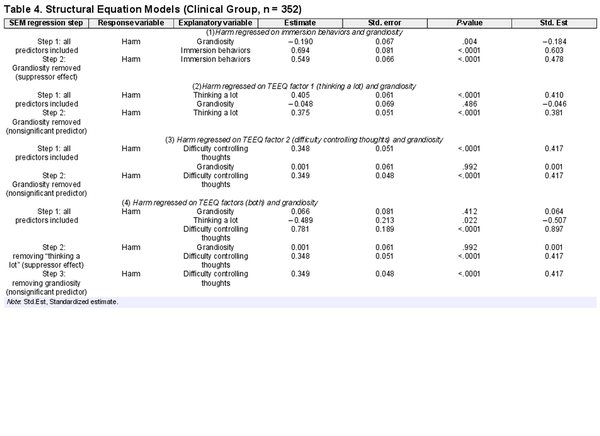
Pair-wise correlations tested whether immersion behaviors and repetitive thinking were associated with grandiosity and harm (table 3). Immersion behaviors (IBQ-EE total) were significantly associated with grandiosity and grandiose delusion conviction, explaining 39.5% and 13.8% of the variance, respectively. TEEQ factors “thinking a lot” and “difficulty controlling thoughts” explained 28.4% and 19.3% of the variance in grandiosity and 19.4% and 11.4% of the variance in grandiose delusion conviction, respectively. The TEEQ factors were strongly correlated and when entered into structural equation models (with grandiosity and grandiose delusion conviction as outcome variables), only “thinking a lot” remained in the models, explaining 20.4% of the variance in grandiosity and 29.6% of the variance in grandiose delusion conviction.
Significant associations were found between immersion behaviors and harm, and the TEEQ factors and harm (table 3). Structural equation models indicated that these associations remained when controlling for grandiosity (table 4).
Pair-wise correlations were used to test the associations between wanting help and grandiosity, grandiose delusion conviction, harm, immersion behaviors, and grandiosity-related repetitive thinking. Wanting help was not significantly associated with grandiosity severity (Spearman’s ρ = 0.04, P = .404) or grandiose belief conviction (ρ = 0.006, P = .914), but was significantly related to harm (ρ = 0.48, P < .0001), immersion behaviors (ρ = 0.25, P < .0001), and grandiosity-related repetitive thinking (“thinking a lot”: ρ = 0.16, P = .002; “difficulty controlling thoughts”: ρ = 0.24, P < .0001).
Post hoc analyses investigated whether the new measures performed similarly in affective and non-affective psychosis diagnoses (Supplementary materials provide full details). There were no statistically significant differences by diagnostic groups for the questionnaire scores. Test–retest and internal reliability scores were similar across diagnostic groups. It was possible to conduct measurement invariance analysis for the TEEQ which demonstrated invariance at the scalar level across diagnoses.
Discussion
Patients frequently reported harm from grandiose beliefs: Over three-quarters reported at least one grandiose-related harmful effect over the past 6 months. Patients identified difficulties across physical, sexual, occupational, social, and emotional domains, the latter two being the most common. Over half of patients wanted help. Therefore, there is a clear route to engagement related to the range of difficulties that grandiose delusions bring in their wake. Notably, awareness of harm and wanting help were independent of the severity of grandiose delusions. Severity of the presentation may well not forestall the successful uptake of treatment.
The majority of patients reported immersion behaviors and grandiosity-related repetitive thinking. Each may plausibly contribute to the persistence of grandiose delusions. Memories of self-performed actions may be stronger compared to imagined actions and thus acting “in role” may provide particularly compelling memories that are perceived as confirmatory evidence for the belief. Alternatively, immersion behaviors may involve withdrawal from others and becoming engrossed in belief-related information, potentially reducing access to disconfirmatory evidence and providing further confirmatory evidence. Repetitive thinking about the grandiose delusion is likely to act by bringing the belief to mind, elaborating the details, and increasing conviction.
Immersion behaviors and grandiosity-related repetitive thinking may also contribute to the occurrence of grandiose-related harm. Why might this be the case? Clearly, in some instances, the immersion behavior is harmful in its own right (eg, trying to fly). Immersion behaviors (eg, blessing people believing one is Jesus) could also lead to social rejection. Being unable to control overwhelming thoughts about one's responsibility for saving the world could lead to emotional distress. Immersion behaviors and repetitive thinking were each associated with wanting help, independent of the severity of grandiosity, providing a further route for engagement in treatment.
The results indicate that many patients would like help, and therefore may well engage with treatments that address their concerns. It will be important for the development of targeted treatments to set out clearly how they will achieve the desired change for patients. Clinicians often anticipate those with the strongest grandiose delusions may be the most difficult to engage in therapy, but this study indicates there should be caution about this assumption. A clear route to engagement is via discussion about the difficulties of grandiose delusions, but there may be a discrepancy between initial clinician and patient perspectives. Clinicians may focus on readily observable and potentially life-threatening forms of harm and physical harm may be the easiest to observe. Indeed, existing research on acting on grandiose delusions focuses almost exclusively on physical harm (typically to others). This, of course, is important but patients endorse this type of harm at relatively low rates. They report social and emotional harms far more frequently, yet these may be less obvious to clinicians. Patients are likely to experience distressing harms that may only be apparent on careful assessment. Similarly, immersion behaviors like “acting in private” and repetitive internal thinking are both difficult for clinicians to directly observe. The questionnaires developed could help facilitate shared awareness between patients and clinicians.
The study has limitations. Primarily, the cross-sectional design means that causal relationships cannot be determined, although the measures developed will enable future longitudinal and interventionist designs to be conducted. Another limitation was the recruitment of the nonclinical group via social media (potentially unrepresentative of the general population) and the representativeness of the participant group (who were predominantly White-British) impacting on the potential generalisability of findings. Our clinical group comprised people who were typically in established contact with mental health services. Many were supported by adult community mental health teams and were likely to have had long-term support from services. Engagement in treatment for grandiose delusions may differ across stages of difficulties and points of contact with services. This would be a relevant area to consider in future research.
The measures had good psychometric properties, although whether the TEEQ factors, “thinking a lot” and “difficulty controlling thoughts”, are truly distinct or may be better considered as a single factor was not entirely clear. Furthermore, it is possible that we did not have an exhaustive set of items for each measure, and aspects of variance may therefore have been missed. The number of participants with a bipolar diagnosis was small, meaning that the factor structure for each questionnaire could not be separately examined by diagnosis. However, total scores on the questionnaires did not differ by diagnosis, although there was an indication that levels of subjective harm associated with grandiose delusions might be higher in the context of bipolar disorder. Measurement invariance across diagnoses was found for the one questionnaire that could be tested in such a way. Although there was no clear evidence of differences in these measures across diagnostic groups, it is still plausible that the influence of different maintenance mechanisms may vary across clinical presentations or across differing belief content. Finally, in this study, we assessed two putative maintenance mechanisms for grandiose delusions, but causation will likely be multi-factorial. Future studies should assess the contributions of multiple factors.
Acknowledgments
We are very grateful to the participants and the Clinical Research Networks in the participating Trusts for giving their time to this research. We also thank Imogen Kilcoyne, David Sher, and Sapphira McBride for their help with data entry. The authors declare that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Isham L, Griffith L, Boylan A, et al. Understanding, treating, and renaming grandiose delusions: a qualitative study. Psychol Psychother. 2021;94(1):119–140. doi: 10.1111/papt.12260.
- 2. Isham L, Sheng Loe B, Hicks A, et al. The meaning in grandiose delusions: measure development and cohort studies in clinical psychosis and non-clinical general population groups in the UK and Ireland. Lancet Psychiatry.2022;9(10):792–803. doi: 10.1016/s2215-0366(22)00236-x.
- 3. Mulder CL, Koopmans GT, Hengeveld MW. Lack of motivation for treatment in emergency psychiatry patients. Soc Psychiatry Psychiatr Epidemiol.2005;40(6):484–488. doi: 10.1007/s00127-005-0913-2.
- 4. Wigman JTW, Vollebergh WAM, Raaijmakers QAW, et al The structure of the extended psychosis phenotype in early adolescence-a cross-sample replication. Schizophr Bull. 37(4):850–860. doi: 10.1093/schbul/sbp154.
- 5. Verdoux H, van Os J, Maurice-Tison S, Gay B, Salamon R, Bourgeois M. Is early adulthood a critical developmental stage for psychosis proneness? A survey of delusional ideation in normal subjects. Schizophr Res.1998;29(3):247–254. doi: 10.1016/S0920-9964(97)00095-9.
- 6. Stefanis NC, Delespaul P, Henquet C, Bakoula C, Stefanis CN, van Os J. Early adolescent cannabis exposure and positive and negative dimensions of psychosis. Addiction.2004;99(10):1333–1341. doi: 10.1111/J.1360-0443.2004.00806.X.
- 7. Ronald A, Sieradzka D, Cardno AG, Haworth CMA, McGuire P, Freeman D. Characterization of psychotic experiences in adolescence using the Specific Psychotic Experiences Questionnaire: findings from a study of 5000 16-year-old twins. Schizophr Bull.2014;40(4):868–877. doi: 10.1093/schbul/sbt106.
- 8. Peralta V, Moreno-Izco L, Calvo-Barrena L, Cuesta MJ. The low- and higher-order factor structure of symptoms in patients with a first episode of psychosis. Schizophr Res.2013;147(1):116–124. doi: 10.1016/J.SCHRES.2013.03.018.
- 9. Appelbaum PS, Robbins PC, Roth LH. Dimensional approach to delusions: comparison across types and diagnoses. Am J Psychiatry.1999;156(12):1938–1943. doi: 10.1176/ajp.156.12.1938.
- 10. Garety PA, Gittins M, Jolley S, et al. Differences in cognitive and emotional processes between persecutory and grandiose delusions. Schizophr Bull.2012;39(3):629–639. doi: 10.1093/schbul/sbs059.
- 11. Bortolon C, Yazbek H, Norton J, Capdevielle D, Raffard S. The contribution of optimism and hallucinations to grandiose delusions in individuals with schizophrenia. Schizophr Res.2019;210:203–206. doi: 10.1016/j.schres.2018.12.037.
- 12. Freeman D, Dunn G, Startup H, et al. Effects of cognitive behaviour therapy for worry on persecutory delusions in patients with psychosis (WIT): a parallel, single-blind, randomised controlled trial with a mediation analysis. Lancet Psychiatry. 2015;2(4):305–313. doi: 10.1016/S2215-0366(15)00039-5.
- 13. Bortolon C, Raffard S. Pondering on how great I am: does rumination play a role in grandiose ideas? J Behav Ther Exp Psychiatry.2021;70:101596. doi: 10.1016/J.JBTEP.2020.101596.
- 14. Gruber J, Harvey AG, Johnson SL. Reflective and ruminative processing of positive emotional memories in bipolar disorder and healthy controls. Behav Res Ther.2009;47(8):697–704. doi: 10.1016/J.BRAT.2009.05.005.
- 15. Qualtrics. 2019. [Online software], USA: provo, Utah. https://www.qualtrics.com.
- 16. Černis E, Evans R, Ehlers A, Freeman D. Dissociation in relation to other mental health conditions: an exploration using network analysis. J Psychiatr Res.2021;136:460–467. doi: 10.1016/j.jpsychires.2020.08.023.
- 17. R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2021. https://www.r-project.org/.
- 18. Revelle W. Psych: procedures for personality and psychological research . Illinois, USA: Northwestern University; 2020. https://cran.r-project.org/web/packages/psych/.
- 19. Rosseel YL. An R package for structural equation modeling. J Stat Softw.2012;48(2):1–36. doi: 10.18637/jss.v048.i02.
- 20. Bartlett A. Note on the multiplying factors for various χ2 approximations. J R Stat Soc.1954;16(2):296–298.
- 21. Kaiser HF. An index of factorial simplicity. Psychometrika.1974;39(1):31–36. doi: 10.1007/BF02291575.
- 22. Ruscio J, Roche B. Determining the number of factors to retain in an exploratory factor analysis using comparison data of known factorial structure. Psychol Assess.2012;24(2):282–292. doi: 10.1037/a0025697.
- 23. Gadermann AM, Guhn M, Zumbo BD. Estimating ordinal reliability for Likert-type and ordinal item response data: a conceptual, empirical, and practical guide response data: a conceptual, empirical, and practical guide. Pract Assess Res Eval.2012;17:3. doi: 10.7275/n560-j767.
- 24. Zumbo BD, Gadermann AM, Zeisser C. Ordinal versions of coefficients alpha and theta for likert rating scales. J Mod Appl Stat Methods.2007;6(1):214–229. doi: 10.22237/jmasm/1177992180.
- 25. Freeman D, Lambe S, Yu LM, et al. Injection fears and COVID-19 vaccine hesitancy. Psychol Med.2021;1:1–11. doi: 10.1017/S0033291721002609.
- 26. Engelkamp J, Zimmer HD. Memory for action events: a new field of research. Memory for Actions. Psychol Res.1989;51:153–157. doi: 10.1007/BF00309142.
- 27. Ullrich S, Keers R, Shaw J, Doyle M, Coid JW. Acting on delusions: the role of negative affect in the pathway towards serious violence. J. Forens. Psychiatry Psychol.2018;29(5):691–704. doi: 10.1080/14789949.2018.1434227.
- 28. Ullrich S, Keers R, Coid JW. Delusions, anger, and serious violence: new findings from the macarthur violence risk assessment study. Schizophr Bull.2014;40(5):1174–1181. doi: 10.1093/schbul/sbt126.
- 29. van Dongen J, Buck N, van Marle H. Unravelling offending in schizophrenia: factors characterising subgroups of offenders. Crim Behav Ment Health. 2015;25:88–98. doi: 10.1002/cbm.1910.